Radiation therapy
![]()
IMRT is a redirect to this article. For another meaning of this abbreviation, see International Human Rights Tribunal.
Radiation therapy (also radiotherapy) is the medical application of ionizing radiation to humans and animals to cure or delay the progression of disease. The radiation may come from devices or from radioactive preparations. Specialties for this particular application of radiation are called radiation medicine and radiation oncology.
The radiation used is mainly gamma radiation, X-rays and electron radiation. In recent years, facilities for treatment with neutrons, protons and heavy ions (often carbon ions) have also been established. Non-ionizing radiation such as microwave and heat radiation, light and UV therapy, and treatment with ultrasound waves are not classified as radiation therapy.
Radiation therapy comprises the treatment of benign and malignant diseases. It is carried out by specialists in radiology or radiotherapy with the assistance of medical-technical radiology assistants and specialised medical physicists. Their activities are subject to the country-specific legislation in radiation protection and the subordinate regulations (cf. Radiation Protection Ordinance) and standards. The actual therapy is preceded by a complex planning process - the radiation planning. Extensive organizational and technical quality assurance measures ensure that irradiation errors can be largely excluded.
According to the training regulations valid in Germany, the field of radiation therapy also includes the medicinal and physical procedures for radiosensitization and enhancement of the radiation effect on the tumor (radioimmunotherapy and radiochemotherapy), taking into account protective measures of healthy tissues.
Application against cancer
Malignant tumors are very often irradiated; often also in combination with other treatment procedures such as surgery and chemotherapy. About every second cancer patient receives one or more radiation therapies. Palliative radiotherapy, for example of bone metastases, and curative treatment, i.e. treatment intended to cure cancer, are about equally common. Neoadjuvant radiotherapy is intended to reduce the size of the tumour for subsequent surgery; adjuvant radiotherapy is intended to secure the result of a previous operation and destroy microscopic tumour nests. Oncological treatment always follows the "log cell kill" principle. Radiotherapy with the intention of healing is designed to destroy the tumour, which often consists of 100 billion cells, down to the last cell. Since individual tumour cells can no longer be detected, the actual success of the treatment only becomes apparent in the months and years that follow. If a tumour forms again at the same site within the follow-up period, it must be assumed that there has been a recurrence.
The treatment decision is based, among other things, on the question of the extent to which the localisation of the tumour to be treated is suitable for radiotherapeutic intervention. Not all tumors are more radiosensitive than the normal tissue surrounding them. One of the causes of lower radiation sensitivity is oxygen deficiency (hypoxia) in the tumor tissue. By means of a combination of fractionation and irradiation technique that is optimally adapted to the tumor biology and the surrounding risk organs, it is now possible to successfully treat even problematically localized and relatively radiation-insensitive tumors. An optimal irradiation technique delimits the tumor region supplied with dose by the steepest possible dose fall-off to normal tissue. Various therapy concepts additionally attempt to increase the radiation sensitivity of tumors with the aid of so-called radiosensitizers (radiation sensitizers).
The curative effect requires a total dose of 20 to 80 Gray, depending on the tumor type and fractionation, administered in one session or spread over several weeks, depending on the treatment regimen. Symptom-relieving treatments for incurable patients can be shorter; for example, bone foci can be treated with a single 8 Gy of pain relief.
With modern radiotherapy procedures, a large number of tumor diseases can be cured today in stage-dependent combination with surgery and chemotherapy, even in advanced stages. Averaged over all tumor types and stages, the chance of cure is about 50 %. Individual tumours such as Hodgkin's disease and seminoma of the testis can almost always be cured. The most common indications for radiotherapy are currently prostate cancer, adjuvant after breast cancer surgery, and for rectal cancer. A particular advantage is the fact that radiotherapy can preserve organs even in situations where the disease is already relatively advanced. The combination of radiotherapy with chemotherapy in the case of cancer of the larynx can be mentioned here in particular. In other tumor diseases, such as prostate carcinoma, surgical procedures and radiotherapeutic procedures compete with each other and can have comparable results. Here, it is the task of the consulting physician to explain to the patient all the advantages and disadvantages of the respective procedures. In this context, it is desirable to have certified tumour centres in which all specialist disciplines are represented and which thus enable the patient to receive comprehensive advice.
Very rarely, an abscopal effect can occur, in which tumor regression up to complete remission is recorded even at sites that were not irradiated. This effect was first described in 1953 and has so far only been reported in isolated cases, such as leukaemia, lymphoma, renal cell carcinoma and malignant melanoma.

Mask for optimal positioning of the head during irradiation
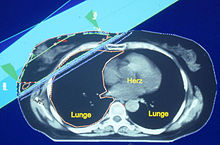
Radiation plan for a breast cancer
Application against benign diseases
→ Main article: Radiotherapy for benign diseases
Numerous chronic inflammatory and degenerative diseases such as heel spurs, tennis elbow, shoulder pain, arthroses of the various joints, vertebral body hemangiomas, induratio penis plastica and others can be treated with radiation therapy. This so-called stimulus radiation far below the tissue-killing dose is free of side effects except for the stochastic risk. Response rates are in the range of 50 to 70 %. The total doses used are in the range of 1 to 20 Gray, which is much lower than the doses that must be used in cancer therapy (20 to 80 Gy). Low-dose radiation reduces the activity of leukocytes and connective tissue precursor cells and decreases the release of cytokines; thus, it inhibits acute and chronic inflammatory processes. Direct inhibition of pain receptors is also suspected. Shoulder pain and heel spurs in particular are readily amenable to radiation therapy. In Germany, about 37,000 patients with non-malignant diseases are irradiated per year, with an increasing tendency.
Search within the encyclopedia