Pulmonary embolism
A pulmonary embolism (LE for short) or pulmonary artery embolism (LAE for short) is a blockage (embolism) of a blood vessel in the lungs or pulmonary circulation. It is usually caused by a blood clot, the so-called thrombus (then it is also called pulmonary thromboembolism or pulmonary artery thromboembolism), more rarely by gas bubbles, for example in a diving accident or by air sucked in during an operation, or by fat (fat embolism, for example by fat from the fatty marrow in bone fractures). Since a pulmonary embolism is potentially life-threatening, first aid measures are always necessary. The falling blood pressure (hypotension) can lead to obstructive shock with circulatory arrest.
Typical symptoms are acute shortness of breath (dyspnoea) and/or chest pain on inhalation. The lack of oxygen (hypoxia) causes a resting pulse of over 100/min (tachycardia), which is accompanied by a high respiratory rate (tachypnoea). The further symptoms are very variable and can include cough (lat.: tussis), blood in the sputum (haemoptysis) and cardiac arrhythmia. In the case of an additional (comorbidity) existing deep vein thrombosis (DVT), the affected leg is usually swollen and painful. Due to the increased pumping resistance in the pulmonary circulation (pulmonary hypertension), the right ventricle is subjected to greater strain (cor pulmonale), which can lead to heart failure.
In addition to the supply of oxygen as required, lysis therapy is carried out to dissolve the thrombus. Intravenous heparin is used to inhibit blood clotting (anticoagulation). After the acute symptoms have subsided, prolonged therapy with perorally administered anticoagulants (see Medical Measures) is usually necessary to prevent recurrence of thrombosis.
In Germany, between 40,000 and 100,000 people die of pulmonary embolism every year. This makes it the third most common cardiovascular disease leading to death after heart attack and stroke.
Origin
In up to 80% of all cases, a blood clot causing a pulmonary embolism develops in the deep veins of the leg or pelvis and travels via the inferior vena cava, the right atrium and ventricle of the heart into both pulmonary arteries. As it progresses, the thrombus becomes lodged and occludes the vessel. The larger the thrombus, the larger the area of the lung behind it that is no longer supplied with blood. Often there are several thrombi which block pulmonary vessels completely or partially at the same time or at intervals.
Both lungs of a patient can also be affected. Amniotic fluid embolisms can also occur
during birth, and fat embolisms in the case of fractures of the long tubular bones (e.g. femur). Even bone marrow embolisms are possible in the lungs. Furthermore, air or other gases (e.g. CO2 during laparoscopy) can enter the venous vascular system during injuries or medical procedures.
Pulmonary embolism is one of the most commonly overlooked causes of death.
The lethality of an untreated severe pulmonary embolism is very high at 30 %. Immediate treatment can reduce mortality to 2-8%.
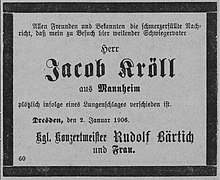
Obituary (1906)
Pathophysiology
The embolus blocks one or more branches of the pulmonary arteries. The larger the internal diameter of the affected vessel, the more serious this becomes. The congestion of blood in front of the thrombus leads to a more or less severe increase in pressure in the pulmonary circulation (pulmonary hypertension) and thus to a strain on the right part of the heart, which may cause it to fail partially or even completely. If the right side of the heart does not fail, there is nevertheless at least a reduction in the amount of blood that can pass through the lungs and reach the left side of the heart. However, the left side of the heart can only pump as much blood as it receives. The consequence of the reduced blood flow is a reduced oxygen supply to the important organs. This can lead to (cardiogenic) shock. Depending on the extent, there may be a lower oxygen content in the blood - hypoxaemia.
A sudden severe pulmonary embolism is called fulminant. The leading symptom is failure of the right heart (right heart failure), accompanied by severe hypoxaemia.
Smaller pulmonary embolisms can also lead to right heart problems. Here, the increase in pressure in the small circulation is not as severe, and the acute survival rate of patients is therefore also significantly higher. In most cases, the thrombi are broken down and the vascular system is thus cleared again. Nevertheless, some patients (especially those with recurrent small pulmonary embolisms) may develop chronic pulmonary hypertension in the further course. This can then be a case of CTEPH.
Following the acute event, an infection of the lung tissue that is no longer sufficiently supplied with blood can lead to a so-called infarct pneumonia. The lung area behind the embolus can infarct, especially after a major embolism with destruction of part of the connective tissue underlying the lung. Despite the high regenerative capacity of the lung tissue, entire areas then die permanently. If the organism survives this, functionless scars develop. If larger areas are affected with a corresponding loss of function, the result is shortness of breath, reduced resilience and often a permanent cough. The facilitated invasion of germs into the initially necrotic, subsequently fibrotically altered - and for antibiotics largely inaccessible - scar tissue also leads later more frequently to pneumonia. The fibrotic remodeling processes also slightly increase the risk of later lung cancer. There is a high rate of late complications, especially with renewed embolisms.
Questions and Answers
Q: What is a pulmonary embolism?
A: A pulmonary embolism is a clot of material that blocks blood from getting to the lungs.
Q: What usually causes a pulmonary embolism?
A: It is usually caused by a blood clot that starts somewhere else in the body and travels to the lungs.
Q: Can a pulmonary embolism be caused by something other than a blood clot?
A: Yes, it can also be caused by clumped cancer cells, fat, or bone.
Q: How rare is it for a woman to get a clot of amniotic fluid while giving birth?
A: It is a rare occurrence for a woman to get a clot of amniotic fluid while giving birth.
Q: What are the symptoms of a pulmonary embolism?
A: Symptoms of a pulmonary embolism include sudden shortness of breath, chest pain, and coughing up blood.
Q: How is a pulmonary embolism treated?
A: Treatment for a pulmonary embolism may include medications to thin the blood, oxygen therapy, and in severe cases, surgery.
Q: Can a pulmonary embolism be prevented?
A: Steps that can be taken to prevent a pulmonary embolism include regular exercise, avoiding prolonged sitting, maintaining a healthy weight, and wearing compression stockings if recommended by a doctor.
Search within the encyclopedia