Osteoarthritis
![]()
This article explains osteoarthritis in humans in general; for other types of osteoarthritis, see Osteoarthritis (disambiguation).
The term osteoarthritis or arthrosis (synonym arthrosis deformans - from ancient Greek ἄρθρον arthron, German 'joint' and Latin deformare 'to mutilate') refers to a degenerative joint disease (joint wear and tear) and is also known as joint wear and tear that exceeds what is normal for age.
The causes are considered to be excessive strain (e.g. increased body weight), congenital or traumatic causes such as malpositioning of the joints or bony deformation due to bone diseases such as osteoporosis. Osteoarthritis can also develop as a result of another disease, such as joint inflammation (arthritis) (secondary osteoarthritis) or be associated with overuse-related effusion formation (secondary inflammatory reaction) (activated osteoarthritis). Osteoarthritis is also called osteoarthrosis (osteoarthrosis) and in the Anglo-American literature osteoarthritis (OA), not to be confused with rheumatoid arthritis (RA), a chronic inflammatory autoimmune disease of the joints.
In principle, all joints can be affected by arthritic changes. In Germany, the disease is most frequently localized in the knee joint. Osteoarthritis is one of the most frequent causes of consultation in a general medical practice. In Germany, about five million people suffer from osteoarthritis. It is the most common joint disease (arthropathy) worldwide.

Medial gonarthrosis MR image of an osteoarthritic knee joint. The osteophytes in the medial (middle) and lateral (side) areas of the joint space and the wear or abrasion of the cartilage layer in the left area of the image are clearly visible. The bone of the tibial plateau in the medial region is compacted, a response to increased mechanical stress. The cartilage layer has lost its cushioning function.
Division
| Classification according to ICD-10 | |
| M15-M19 | Osteoarthritis |
| M47 | Spondylosis (including osteoarthritis or osteoarthrosis of the spine, degeneration of the articular surfaces) |
| ICD-10 online (WHO version 2019) | |
Basically, a distinction is made between primary and secondary osteoarthritis.
In primary osteoarthritis, a biological inferiority of the cartilage tissue of unclear cause is assumed. Secondary arthrosis is caused by mechanical overload (e.g. in hip joint dysplasia), inflammatory changes (e.g. in arthritis) or metabolic disorders (e.g. in chondrocalcinosis). The frequency distribution of both forms is controversially discussed.
In osteoarthritis, initial cartilage damage leads to changes in the bone as the disease progresses:
- In stage 1, there is roughness and thinning of the cartilage layer, tangential fissures appear.
- In stage 2, hyaline cartilage is replaced by granulation tissue and inferior fibrocartilage. Pseudocysts of necrotic cartilage and bone tissue (boulder cysts) form.
- In stage 3, ulcerations already occur, the connective tissue and the chondrocytes proliferate.
- In stage 4, the bone plate of a joint flattens. In order to absorb the pressure on the joint nevertheless, marginal ridges form on the bone (osteophytes).
Causes
Basically, osteoarthritis is also differentiated according to its cause. Arthrosis alcaptonurica is caused by an increased deposition of homogentisic acid in joints with pre-existing alcaptonuria. In haemophilic arthrosis, regular intra-articular bleeding is present in haemophilia (haemophilic joint). Arthrosis urica is caused by the mechanical impact of urate crystals (uric acid) on healthy cartilage.
The classic cause of arthrosis is joint dysplasia. Taking the hip as an example, it becomes clear that the zone subject to the greatest mechanical load in a physiological hip position represents a significantly larger area than in a dysplastic hip. However, the loads caused by the forces acting on the joint are largely independent of the joint shape. They are essentially distributed over the main loading zone(s). As a result, a smaller zone will have a higher compressive load than a larger one. The biomechanical pressure load on the articular cartilage is thus greater in a dysplastic hip than in a physiological hip. This law is generally considered to be the cause of the frequent occurrence of arthritic changes in weight-bearing joints that deviate from the ideal anatomical shape.
If the consequences of an injury are responsible for premature wear, this is referred to as post-traumatic arthrosis. Other causes of secondary osteoarthritis are discussed as mechanical, inflammatory, metabolic, chemical (quinolone antibiotics), trophic, hormonal, neurological and genetic. In most cases, the development of osteoarthritis is considered idiopathic, that is, without a currently identifiable cause.
Medicinal causes of osteoarthritis can be, for example, antibiotics from the class of gyrase inhibitors (fluoroquinolones such as ciprofloxacin, levofloxacin). These drugs cause complexation of magnesium ions in poorly vascularized tissues (hyaline articular cartilage; tendon tissue), resulting in irreversible damage to connective tissue. This damage is usually more pronounced in children and adolescents during the growth phase. Tendopathies and arthropathies are known side effects of this class of drugs. In adults, according to information from independent pharmacologists and rheumatologists, these antibiotics lead to accelerated physiological degradation of hyaline articular cartilage. Long-term treatment with phenprocoumon can also promote arthrosis due to a decrease in bone density during stresses on the inner joint structure.
In addition to age, mechanical overload, (micro)trauma, destabilization of the joints caused by loss of locking mechanisms, and genetic factors are known risk factors for osteoarthrosis. However, neither the origin of osteoarthritis nor the possibilities for intervention have been fully clarified.
In a joint affected by osteoarthritis, the content of nitric oxide is increased. Something similar could be observed through mechanical irritation of cartilage tissue. Mechanical forces are probably causally involved in the development of osteoarthritis.
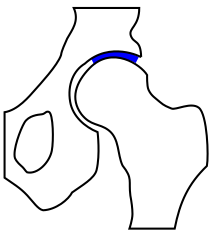
Hip joint - the main mechanical loading zone is shown in blue.
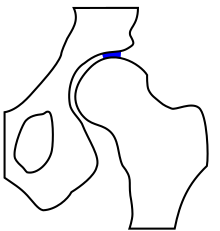
Hip joint dysplasia - the main mechanical stress zone is significantly reduced compared to the normal variant.
Questions and Answers
Q: Who is most commonly affected by osteoarthritis?
A: Osteoarthritis normally affects older people.
Q: What happens to the joint surface in osteoarthritis?
A: The joint surface wears away in osteoarthritis.
Q: What happens when the joint surface wears away?
A: When the joint surface wears away, it sheds particles which stimulate the joint lining to produce fluid. This causes the joint to swell.
Q: What happens when the joint cartilage wears away in osteoarthritis?
A: When the joint cartilage wears away in osteoarthritis, the core of the bone becomes exposed.
Q: What happens when the exposed bone rubs against other exposed bone in osteoarthritis?
A: When the exposed bone rubs against other exposed bone in osteoarthritis, it causes pain and discomfort.
Q: What is the cause of the joint swelling in osteoarthritis?
A: The shedding of particles due to the joint surface wearing away stimulates the joint lining to produce fluid, causing joint swelling.
Q: What would be a likely symptom of osteoarthritis?
A: Pain and discomfort due to bone-on-bone contact when joint cartilage wears away.
Search within the encyclopedia