Myocardial infarction
![]()
This article or section needs revision: The article is out of date in important respects and needs urgent updating. See discussion page. --Saidmann (discussion) 22:18, 22 May 2020 (CEST)
Please help improve it, and then remove this tag.
Myocardial infarction or (more precisely) myocardial infarction, also called coronary infarction, is an acute and life-threatening event resulting from a disease of the heart in which a coronary artery or one of its branches becomes displaced or more constricted. Abbreviations commonly used in human medicine are HI, MI (myocardial infarction) or AMI (acute myocardial infarction).
It is a persistent circulatory disturbance (ischemia) of parts of the heart muscle (myocardium), which in most cases is caused by blood clots in an arteriosclerotically altered constriction of a coronary vessel. The leading symptom of myocardial infarction is a sudden, persistent and usually severe pain in the chest area, which may radiate mainly to the left side into the shoulders, arms, lower jaw, back and upper abdomen. It is often accompanied by sweating/cold sweats, nausea and possibly vomiting. In about 25% of all heart attacks, there are only minor or no symptoms (so-called silent heart attack). In the acute phase of a heart attack, dangerous cardiac arrhythmias frequently occur; even minor infarctions often lead to sudden cardiac death via ventricular fibrillation. About 30 % of all deaths in heart attacks occur before any lay help or medical therapy.
This article deals mainly with myocardial infarction in humans; myocardial infarction in animals is described separately at the end.
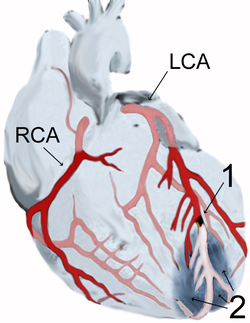
Myocardial infarction of the anterior wall apex (2) after occlusion (1) of the anterior descending branch (LAD) of the left coronary artery (LCA), schematic diagram
Epidemiology
Myocardial infarction is one of the main causes of death in industrialized nations. The incidence is about 300 infarctions per 100,000 inhabitants per year in Austria/Germany (in Japan < 100; Mediterranean, Switzerland, France < 200; 300 to 400 in Scandinavia; 400 to 500 in England, Hungary), in Germany about 280,000 people suffer a heart attack every year. According to the cause of death statistics of the Federal Statistical Office, more than 49,000 people died in Germany in 2015 as a result of an acute myocardial infarction. This means that acute myocardial infarction has always ranked second among the causes of death in Germany since 1998. Both the absolute number of deaths as a result of a heart attack and the relative frequency have been steadily declining in Germany for years (see table).
| Year | absolute number | Male | female |
| 2000 | 67.282 | 36.458 | 30.824 |
| 2001 | 65.228 | 35.473 | 29.755 |
| 2002 | 64.218 | 34.907 | 29.311 |
| 2003 | 64.229 | 34.679 | 29.550 |
| 2004 | 61.736 | 33.348 | 28.388 |
| 2005 | 61.056 | 32.973 | 28.083 |
| 2006 | 59.938 | 32.471 | 27.467 |
| 2007 | 57.788 | 31.195 | 26.593 |
| 2008 | 56.775 | 30.559 | 26.216 |
| 2009 | 56.226 | 30.934 | 25.292 |
| 2010 | 55.541 | 30.651 | 24.890 |
| 2011 | 52.113 | 28.621 | 23.492 |
| 2012 | 52.516 | 28.951 | 23.565 |
| 2013 | 52.044 | 28.991 | 23.053 |
| 2014 | 48.181 | 27.188 | 20.993 |
| 2015 | 49.210 | 27.835 | 21.375 |
| 2016 | 48.669 | 28.130 | 20.539 |
| 2017 | 46.966 | 27.130 | 19.836 |
| 2018 | 46.207 | 26.884 | 19.323 |
Heart attacks occur significantly more often in socially poorer neighbourhoods. In addition, in contrast to patients from more socially privileged districts, patients from these neighbourhoods are younger and have a higher risk of dying within one year after the heart attack.
Play media file Video describes the mechanism of heart attacks (English)
Diagnostics
Current and newer diagnostic methods
The diagnosis of myocardial infarction is made when one of the so-called "biomarkers" (preferably cardiac troponin, alternatively CK-MB) is elevated in the blood and at least one of the following criteria is fulfilled:
- typical ECG changes or
- typical chest pain or
- recent intervention on a coronary vessel (for example, PTCA).
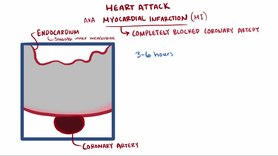
However, the blood concentration of the biomarkers troponin and CK-MB increases only after three to six hours, so that a reliable diagnosis was previously only possible after four to six hours.
According to recent studies, a faster and more specific diagnosis can now be made promptly using the newly discovered cardiac marker glycogen phosphorylase BB (GPBB). GPBB can be used to diagnose a heart attack as early as the first hour, reducing the risk of irreversible damage to heart tissue.
In this acute phase, the most important examination procedure is an ECG obtained as quickly as possible. If ST-segment elevations are detected, an infarction is assumed with a diagnostic certainty of more than 95% and the appropriate treatment is initiated as soon as possible.
If, on the other hand, the ECG shows ST-segment depression or no changes, infarction cannot be excluded or confirmed with certainty on the basis of the biomarkers until six hours after the onset of symptoms. If there is diagnostic uncertainty at this stage, the detection of wall motion abnormality on echocardiography can help to better assess the likelihood and extent of an infarction.
Differential diagnosis
Because of the potentially far-reaching consequences, the suspected diagnosis of myocardial infarction was often made in the past; in the acute situation, the differential diagnoses of pneumothorax, pulmonary embolism, aortic dissection, pulmonary edema of another cause, herpes zoster, stress cardiomyopathy, Roemheld syndrome, cardiac neurosis, or biliary colic then had to be considered. Only about 32% of patients with suspected infarction actually had a heart attack. Today, the term infarction is usually avoided until it is definitively proven, and the term acute coronary syndrome is used instead to reflect the frequent diagnostic uncertainty in the first few hours.
Infarct diagnosis is also subject to possible errors: in some patients (0.8% in one study), especially in elderly patients and those with diabetes mellitus, the infarct is not correctly detected even in hospital.
An unusual confusion of symptoms was observed in a (rather rare) case of consumption of honey from the Turkish Black Sea coast (see Honey#Toxins in honey and toxic honeys).
Questions and Answers
Q: What is an acute myocardial infarction?
A: An acute myocardial infarction, also known as a heart attack, occurs when a blood vessel in the heart suddenly becomes blocked and cannot supply enough oxygen to part of the heart.
Q: What is Angina Pectoris?
A: Angina Pectoris is chest pain that results from the lack of oxygen-rich blood in the heart due to an occluded artery.
Q: What does "myocardial infarction" mean?
A: Myocardial infarction means "infarction (muscle death) in the heart muscle."
Q: Is a heart attack a medical emergency?
A: Yes, a heart attack is considered a medical emergency and requires immediate attention.
Q: How long does someone have to get treatment for their heart attack?
A: It is important for someone who has had a heart attack to receive treatment within the first hour of their attack for optimal results.
Q: What happens if there isn't enough oxygen getting to part of the heart?
A: When there isn't enough oxygen getting to part of the heart, it can cause ischemia which can lead to chest pain called Angina Pectoris.
Search within the encyclopedia