Menstrual cycle
The menstrual cycle, menstrual cycle or female cycle is in humans a monthly (about every 20 to 35, on average every 27 days) occurring process in the body of the woman, which takes place from puberty (with menarche) to menopause (with menopause) about 400 times and is characterized by hormonal changes aimed at creating favorable conditions for fertilization and pregnancy at various physical levels, primarily in the ovary (see also ovarian cycle) and at the uterus. The first day of menstruation has been defined as the beginning of a menstrual cycle because bleeding is the most obvious and visible symptom within the cycle. According to the definition, the cycle ends on the day before the onset of bleeding.
In the course of a cycle, if no conception has taken place, the endometrium is shed (desquamation) and then rebuilt (proliferation and secretion). In the meantime, an egg has matured in one of the two ovaries (follicle maturation), which reaches the fallopian tube at ovulation and is made available for fertilisation during the next 12-18 hours. These processes are controlled by the hypothalamus, pituitary gland and ovary via various hormones: oestrogen and progesterone trigger the changes in the lining of the uterus. Chemically modified oestrogen and progesterone analogues are the main components of contraceptive pills. They are used to trick the body into thinking that it is in the luteal phase, when no further egg maturation or ovulation takes place. The body's own cycle with egg maturation, ovulation and luteal phase is replaced by a cyclical sequence of hormone administration from the outside.
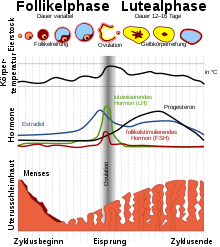
The cycle is divided into two phases:
- The period between the onset of menstruation and the next ovulation is called the desquamation and proliferation phase or follicular phase or egg maturation phase and is variable in duration. It can last a few days, but also many weeks.
- The phase between ovulation and the start of menstruation is called the secretory or luteal phase. It lasts, relatively constant, between ten and 16 days. If it lasts less than ten days, it is referred to as "luteal weakness" or "luteal insufficiency". In such a cycle, fertilisation can take place, but the fertilised egg cannot implant. A luteal phase over 16 days indicates the onset of pregnancy.
Cycles that last 23 to 35 days are considered "normal". 5% of cycles in healthy women last longer than 35 days.
The first menstrual cycle in a woman's life begins before the first menstrual period (menarche) with the preparation of the first ovulation, the last one ends with the last menstrual period (menopause). Between the first and the last, one cycle follows the previous one, if this sequence is not interrupted by pregnancy, by certain diseases or by hormonal contraception.
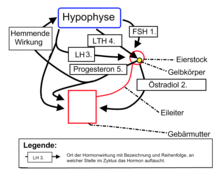
Hormones occurring during the cycle with site of action
Schematic representation of the ovarian cycle
Processes prior to sexual maturity
The menstrual cycle continues a development that begins in the human embryo as early as the 3rd week: Primordial germ cells migrate into the female gonadal anlage, differentiate in the course of oogenesis into oogonia and partly further into oocytes, the actual oocytes, which enter the 1st maturation division before the birth of the girl. These oocytes, as so-called primary oocytes, form the so-called primordial follicle together with the epithelium surrounding them.
Further development is now interrupted
until the onset of puberty and the oocytes enter a resting stage, the dictyotene. During this dormant stage, most oocytes perish again. At the time of menarche - the first menstrual period - about 400,000 of the original 700,000 to 2 million primordial follicles are still present.
The phases of the menstrual cycle
With the entry into sexual maturity begins the fertile phase of the woman.
Desquamation and proliferation phase, follicular phase
The first day of menstruation marks the beginning of a new cycle. In the first phase of the cycle, the old mucous membrane layer of the uterus is shed and washed away with menstruation (desquamation phase) and, after the end of bleeding, is rebuilt under the influence of the oestrogen produced in the ovary (proliferation phase). At the same time, an ovarian follicle containing the egg matures in the ovary (follicular phase):
Under the influence of follicle-stimulating hormone (FSH), 5 to 15 primordial follicles grow in each ovary at the beginning of the individual ovarian cycle. In the process, both the follicle cells and the theca cells of the ovary multiply.
The proliferating follicle cells produce progesterone and release it into the follicular cavity, which supports egg maturation. The granulosa cells produce estrogen, which enters the bloodstream and, among other things, brings the uterine lining into the proliferation phase (preparation for implantation).
A primordial follicle grows and matures via primary and secondary follicles to become a tertiary follicle. As a rule, only one of the primordial follicles develops into a mature tertiary follicle ready to jump, the others perish and become connective tissue.
With the follicle rupture, an egg cell is now ejected, which after many years of resting in the dictyotene stage has now completed the first maturation division.
The progesterone-producing follicle cells of Graaf's follicle are now infused with blood vessels, causing a rise in progesterone in the blood.
Ovulation and fertile phase of the cycle
Ovulation (also called ovulation or follicular leap) itself is not called a phase, but merely marks the change between the follicular and corpus luteum phases.
Depending on the length of the follicular maturation phase, ovulation occurs at different times, in only 25% of cases on the 14th or 15th day of the cycle. In 60 % of cases ovulation occurs after the 14th day of the cycle, in 5 % already on the 11th day of the cycle or even earlier. Just before ovulation, the estrogen concentration in the blood is at its highest. Although there are two ovaries, usually only one egg is developed per cycle. Which ovary becomes the follicle supplier is essentially random, because there is no right-left coordination. When the level of follicle stimulating hormone (FSH) rises, the maturation of the follicle is stimulated. The follicle secretes inhibin, which prevents the FSH level from rising and thus prevents another follicle from maturing. Thus, it varies each time whether the left or right ovary produces the follicle; after the loss of one ovary, the other is usually able to perform the duties on its own. In some women, follicular rupture is accompanied by a characteristic pain called mittelschmerz, which can last for several hours. The egg is about 0.1 mm in diameter. After ovulation, the egg can be fertilized by a sperm in the outer third of the fallopian tube for 12-18 h. If this does not happen, it dies. If this does not happen, it dies and dissolves. If it is fertilised, it travels through the fallopian tube to the uterus during the next 3-4 days.
The oestrogens produced in the ovary during the follicular phase not only build up the lining of the uterus but also cause the formation of the so-called cervical mucus in the glands of the cervix. This cervical mucus enables the sperm to survive in the woman's body for up to 5 days, so that - together with the egg's ability to fertilise for just under one day - we speak of a "fertile window" of 6 days. Various natural family planning methods attempt to determine this fertile window as accurately as possible using body signs such as cervical mucus and basal body temperature.
Corpus luteum or luteal phase, secretory phase and infertile phase of the cycle
After ovulation, the cells of the Graafian follicle form the corpus luteum (corpus luteum) through the action of luteinising hormone (LH, lutropin), which also produces the hormone progesterone under the influence of LH and causes various changes:
In the uterine mucosa, the combination of estrogen and progesterone effects leads to a further expansion of the vascular supply and to a release of secretion containing nutrients from the glands of the mucosa (decidualization). The mucous membrane is prepared for the implantation (nidation) of the fertilised egg about one week after ovulation.
At the cervical glands in the cervix, progesterone causes the cervical mucus to thicken, forming a plug of mucus that is impenetrable to sperm.
At the hypothalamus and pituitary gland, progesterone causes the release of FSH to stop via a negative feedback mechanism, thus preventing any further maturation of the egg and renewed ovulation during the luteal phase. Since neither sperm nor a fertilisable egg are present in the female body, no (renewed) fertilisation can occur during the luteal phase, it is an infertile cycle phase.
If pregnancy does not occur, the corpus luteum in the ovary perishes and becomes a white body (corpus albicans) through scarring. Progesterone production dries up. Without the hormonal support, the mucous membrane cannot be maintained and is shed, bleeding occurs, which also marks the beginning of the next cycle. Due to the drop in progesterone, the negative feedback mechanism is reversed and a new ovulation can begin. The
corpora albicantia finally consist only of connective tissue and give the senile ovary its scarred appearance. The process described here is repeated about 400 times until the last menstrual period, the menopause.
Pregnancy and birth
If fertilization occurs, the egg has a 25 to 30 percent chance of nesting in the uterine wall (nidation) and pregnancy begins. The ovarian cycle is interrupted, superfetatio cannot occur - the new fertilization of an egg with an already existing pregnancy, which, however, is also almost impossible due to the nature of the cervical mucus during pregnancy and its impenetrability for sperm. Depending on whether and how long breastfeeding took place, the ovarian cycle resumes after birth when the concentration of the hormone prolactin, which promotes milk production, has fallen to such an extent that it no longer suppresses FSH and LH release. After pregnancy, ovulation occurs in 50% of breastfeeding women before menstruation recurs, so women can also become pregnant again before their first menstrual period. Breastfeeding can suppress ovulation, but the effect is not certain and provides protection against re-pregnancy only under special, very strictly prescribed conditions; see: Breastfeeding and Contraception and Lactational Amenorrhea Method.
Bleeding
→ Main article: Menstruation
During a regular menstruation of normal duration (three to five days) and strength (called eumenorrhea), about 30 to 60 milliliters of blood are lost (values between 10 and 80 ml are considered normal, the bleeding maximum is usually on the second day). Depending on the author, the threshold for hypermenorrhoea (unhealthily heavy menstruation) is given as 150 ml or 200 ml. The blood is prevented from clotting by the enzyme plasmin, which is contained in the lining of the uterus. In many women menstruation is accompanied by various unpleasant symptoms, so-called menstrual cramps (medically dysmenorrhoea), which can also precede menstruation. They are caused by the hormones involved and the contracting uterus. However, some women also experience the time of menstruation as positive, accompanied by an increased body awareness.
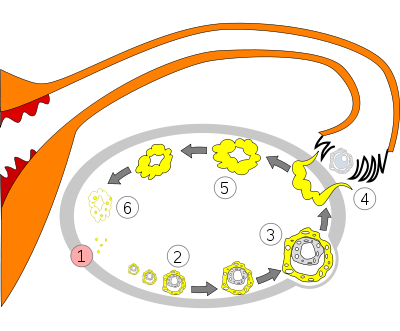
Processes within the ovary during the menstrual cycle: 1 Menstruation2 Maturing follicle3 Mature follicle4 Ovulation5 Corpus luteum6 Regression of the corpus luteum
Questions and Answers
Q: What is the menstrual cycle?
A: The menstrual cycle is a process that adult women go through during which the women's ovaries create a mature ovum (egg), and the woman's body prepares for pregnancy by thickening the walls of the uterus.
Q: How often does the menstrual cycle repeat?
A: The menstural cycle repeats every 28 days while women are not pregnant.
Q: What happens if a woman does not become pregnant during the menstrual cycle?
A: If a woman does not become pregnant during the menstrual cycle, the egg and the lining of the uterus come out of the woman's body during menstruation.
Q: What are the four major hormones that control the menstrual cycle?
A: The four major hormones that control the menstrual cycle are follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone.
Q: Why do these hormones control the menstrual cycle?
A: These hormones prepare the uterus to receive a fertilized egg and control its development.
Q: How many stages are there in the menstrual cycle?
A: There are three stages in the menstrual cycle: the follicular stage, ovulation, and the luteal (or premenstrual) stage.
Q: When will the menstrual cycle stop?
A: The menstrual cycle will stop if the woman gets pregnant (if a fertilized egg implants itself into the lining of the uterus).
Search within the encyclopedia