Lung
![]()
The title of this article is ambiguous. For other meanings, see Lung (disambiguation).
The lung (Latin pulmo) is a paired organ of respiration; its purpose is to provide a large surface area for gas exchange between air and blood. True lungs are found in many air-breathing vertebrates, such as most land-living vertebrates and some fishes, such as the lungfish. Humans have two lungs (pulmo dexter for the right lung and pulmo sinister for the left), which are also called lungs or pulmonary hemispheres in German. The left lung is divided into two lobes and the right lung into three lobes. Gas exchange takes place at the level of the alveoli, which are the end structures of branched airways connected to the trachea.
Fresh air is brought to the blood-air barrier by inhalation and exhalation; this is not a performance of the lungs themselves (the mammalian lung has no musculature), but of the diaphragm and intercostal muscles. The pleural space, whose fluid film transmits forces via adhesion and cohesion, mediates the displaceable mounting of the lungs in the thorax; since they have a tendency to contract when it expands, there is a negative pressure in the pleural space.
The lungs develop embryonically as outpouchings of the foregut (see gill gut) and initially resemble glands. The amphibians have simple lungs; they are sac-shaped and smooth-walled or only slightly chambered. They are much more strongly chambered in the reptiles. In birds they are relatively small, but because of the additional air sacs they are also much more complicated in construction. The lungs of mammals are similar to those of reptiles.
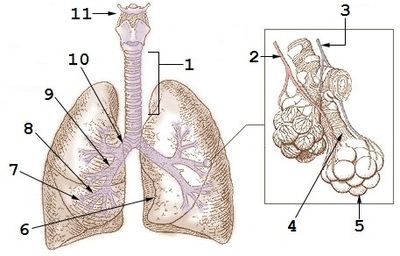
Schematic of human lungs. 1: trachea, 2: pulmonary vein, 3: pulmonary artery, 4: alveolar duct, 5: alveoli, 6: cardiac incision, 7: small bronchi, 8: tertiary bronchus, 9: secondary bronchus, 10: main bronchus, 11: hyoid bone.
Language
Etymology
The German word lunge, via its Old High German form lunguna, ultimately derives from the Indo-Germanic root *lengu̯h 'light (in movement and weight)', so that the original meaning as 'the light one' can be assumed. Linguists explain the naming by the phenomenon, noted long ago, of the lungs of a slaughtered animal being the only organ floating on top of the water. The medical Latin technical term pulmo goes back to an alternative spelling of the Greek word for lung: Ancient Greek πλεύμων (pleumon), whose standard spelling πνεύμων (pneumon) underlies, among other things, the word pneumonia (= pneumonia).
The lungs of mammals
Both lungs of mammals, also called lungs, are movably embedded in the chest cavity (thorax). More or less deep incisions divide the lungs into lobes (lobi). The surface of the lungs is covered by a smooth lining (tunica serosa), which in the thoracic cavity is called the pleura and is subdivided into the lung pleura (pulmonary pleura) and the pleura of the ribs (thoracic pleura). Between the pleural covering of the lung and the pleural lining of the thoracic cavity lies the pleural space, a space filled with a small amount of fluid, in which there is negative pressure.
Structure of the human lung
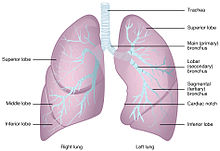
The human lungs, as typical mammalian lungs, consist of a right lung (right lung) and a left lung (left lung). Each lung is divided by furrows into so-called lung lobes. The right lung is divided into three lobes (upper lobe or lobus ventrocranialis, middle lobe or lobus medius and lower lobe or lobus dorsocaudalis), the left lung into only two lobes (upper lobe and lower lobe). The lung lobes in turn are subdivided into lung segments. The designation here is according to the allocation to the supplying bronchial branch. 10 segments are found in the right lung (pulmo dexter). In the left lung (Pulmo sinister) there are only 9 segments, because the 7th segment is missing. The left lung is slightly smaller than the right lung because the heart takes up some space on the left side. Here, the right lung upper lobe consists of the apical, posterior, and anterior upper lobe segments, and the middle lobe (right side only) consists of the lateral and medial middle lobe segments (segments 4 and 5). This is followed by the apical lower lobe segment (segment 6) and the four basal lower lobe segments on the right (mediobasal, anterobasal, laterobasal, posterobasal). On the left side, the upper lobe consists of segments 1 to 3, naming as in the right upper lobe, and the two lingula segments (4, 5) (superior and inferior lingula segments). This is followed by the apical lower lobe segment (segment 6) and the three basal lower lobe segments: anterobasal, laterobasal and posterobasal (segments 8 to 10). The mediobasal segment is missing.
That the functional lung unit is not the lung lobe but the lung segment was recognized by the American surgeon Richard H. Overholt in Boston.
The lungs lie in the thoracic cavity. At the top, the tip of the lung protrudes about 1-2 cm above the collarbone; at the bottom, the lung rests on the diaphragm, the position of which is very variable and depends primarily on the breathing position and the body position (higher when lying down than when sitting). Roughly speaking, it can be said that in the resting breathing position the edges of the lungs come to rest at the level of the 6th rib on the abdominal side, at the level of the 8th rib on the side and at the level of the 10th rib on the dorsal side. This difference results from the oblique diaphragmatic attachment line.
The left lung is generally smaller because the heart rests on it for the most part. Because of this and the splitting of the trachea into the main bronchi, so that the left trachea-bronchus angle is smaller than the right, the right lung is generally better ventilated. The angle included by the trachea and right main bronchus is greater than that between the trachea and left main bronchus. This has consequences in the aspiration of foreign bodies: these usually enter the right main bronchus. The lung volume of an adult human being is on average 5 to 6 litres.
Feinbau
The tissue of the lungs can be divided into an air-conducting part and a part where the actual gas exchange takes place. The air-carrying bronchi end in blind-ending sacs, the alveoli. The gas exchange takes place in these.
The entirety of the air-conducting system is called the bronchial system (bronchial tree). From the inside to the outside, different layers are found. At the beginning, the epithelium (covering tissue) still consists of multi-rowed, highly prismatic ciliated epithelium, as in the trachea, but closer to the alveoli the structure simplifies, and in the bronchioles single-layered iso- or highly prismatic ciliated epithelium predominates. The underlying lamina propria contains smooth muscle, the proportion of which increases towards the alveoli. Furthermore, it contains a large number of elastic fibres as well as mucous and serous glands, whose outlets open into the bronchus and which cover the mucosal surface with a protective film. On the very outside, hyaline cartilage is found in the large bronchi, which ensures that the airways remain open. The smaller the diameter of the bronchi, the smaller the proportion of cartilage mass, until only small islands are found.
The arteries and veins of the pulmonary circulation and the nerve fibres of the pulmonary plexus also run together with the bronchi.
Gas exchange
See also: Pulmonary circulation
The oxygenation of the blood and the release of CO2 takes place in the alveoli. These approximately 300 million sac-like dilations (in adult humans) have a diameter of about 200 μm. The area they form is called the respiratory area. The alveoli consist of the small alveolar cells or pneumocytes type I, which may be less than 0.1 micrometer thick and form the epithelium of the alveoli, and the large alveolar cells or pneumocytes type II, which produce surfactant. The anti-alelectase factor reduces the surface tension against collapse. Furthermore, alveolar macrophages (scavenger cells) are found, which originate from the blood and phagocytize dust (dust cells) or take up hemosiderin, a degradation product of the blood pigment hemoglobin, after bleeding (heart cells).
Between air and blood there is a three-layer partition, the blood-air barrier. It is formed by the epithelium of the alveoli, the epithelial and endothelial basement membrane and the endothelium of the capillaries and is between 0.1 and 1.5 μm thick.
Since the intercellular junctions of the capillary endothelium are more permeable to fluid than those of the alveolar cells, fluid can leak into the connective tissue in heart failure, leading to interstitial edema (pulmonary edema).
The connective tissue between the bronchi and alveoli contains the branches of the pulmonary arteries and veins. The branches of the pulmonary artery carry the blood to the alveoli. Lymph drainage occurs via the pulmonary lymph nodes (Nll. pulmonales) and then into the tracheobronchial lymph nodes (Nll. tracheobronchiales).
Blood vessels
The blood supply to the wall of the alveoli is provided by the capillaries of the pulmonary circulation (vasa publica, 'public vessels'). The remaining tissue, i.e. the area surrounding the bronchi and the connective tissue septa, is supplied by bronchial vessels (rami bronchiales, vasa privata, 'own vessels') from the systemic circulation. The rami bronchiales for the left lung (usually two) arise directly from the thoracic aorta. The bronchial branches for the right lung arise from a trunk of the third or fourth posterior intercostal artery. Both vascular systems often form anastomoses in the periphery.
Most bronchial veins empty into the pulmonary veins, whereas the bronchial veins near the hilum empty into the azygos vein on the right and the hemiazygos vein on the left. Blood entering the pulmonary veins from the bronchial arteries, together with blood from coronary vessels opening into the left heart (vv. cardiacae minimae), causes a small, physiological right-to-left shunt. Together with functional short circuits in the pulmonary circulation (perfusion of non-ventilated parts of the lungs), this explains the lower partial pressure of oxygen in the arteries of the systemic circulation compared to the alveoli.
Ontogenetic development
See also: Blood circulation#The blood circulation of mammals before birth
The lung is the only organ whose ability to function while the fetus is still in the womb is not necessary for survival. Only after birth (but then within seconds) it assumes its main function. Nevertheless, it plays an important role before birth: the lungs produce up to 15 ml of amniotic fluid per kg of body weight every day.
The development of the lung begins about day 30 with the formation of the lung bud from the ventral (abdominal) part of the foregut. As with the latter, the epithelium lining the lung and its air-conducting apparatus (larynx, trachea, bronchi) is of entodermal origin. In contrast, the muscular and cartilaginous tissue originates from the mesoderm surrounding the intestinal tube.
The lung bud then divides further into a right and a left branch (the later main bronchi). Further, the right branch divides into three more branches, the left branch into two. Each of these five further branches later forms a lobe of the lung (lobus pulmonis). From the 5th to about the 17th week, the entire later air-conducting part of the lungs is laid out, i.e. the further branches of the bronchi up to the bronchioli terminales. Initially, this is lined only by highly prismatic epithelium, but from the 13th week of pregnancy the first ciliated epithelial cells are found. Cells of the epithelium begin to produce amniotic fluid.
From the 16th to the 26th week, the ends of the bronchioli terminales form the canaliculi, from which the lung parenchyma emerges. The latter is the functional tissue of the lung in which gas exchange takes place after birth. A cell type typical for the lung parenchyma are pneumocytes type II, which secrete surfactant. Some type II pneumocytes differentiate into type I pneumocytes, and capillaries invade the developing lung parenchyma. The wall of the capillaries and the membrane of the type I pneumocytes later form the blood-air barrier when surfactant (→ lung maturation) is formed from the 28th week of gestation.
In the last trimester of pregnancy, the canaliculi reform into further branches, which ultimately end up as sacculi blind. All these branches of the lung parenchyma are lined with type I and type II pneumocytes. The walls of the sacculi and, in some cases, of the upstream branches bulge out to form hemispherical alveoli. Like the previous processes, this greatly increases the surface area covered by parenchyma. Disturbances in this development can lead to lung malformation. A newborn has far fewer alveoli than an adult. The formation of the alveoli is not completed until infancy.
Until shortly after birth, the lungs contain amniotic fluid; then the muscular apparatus at the ribs and diaphragm increases the volume of the chest and, as a result of the greater air pressure outside, air flows into the bronchi and penetrates the alveoli. The surfactant reduces the surface tension of water, thus preventing respiratory distress syndrome in the newborn. The fluid present is absorbed and carried away via the blood rather than expelled or coughed up. An initial cry confirms the air filling the newborn's lungs. The bypass circuits close.
See also: Breathing drive
Physiology of inhalation and exhalation
→ Main article: Pulmonary ventilation
Breathing usually begins with the intercostal muscles or diaphragm when inhaling (inspiration). The diaphragm is the strongest inspiratory muscle; as it contracts, it flattens and pushes the abdominal and pelvic viscera caudally (tailboneward), increasing thoracic volume. During thoracic breathing, the musculi intercostales externi (external intercostal muscles) contract. This raises and expands the thorax, causing co-expansion of the lungs, which, themselves covered by the visceral (or pulmonary) pleura, communicate with the parietal pleura of the chest via the pleural cavity (cavitas pleuralis). This reduces the pressure in the lungs. After major exertion, other respiratory muscles can be used to facilitate breathing, e.g. the small and large chest muscles. Athletes take advantage of this after an intensive race, for example, by supporting themselves with their arms against a wall: their arms are then fixed (punctum fixum), and thus the chest muscles do not pull the arms towards the chest, but vice versa, the chest towards the arms, the ribs are lifted, and the lungs fill with air. However, according to the pressure-volume relationship (Boyle-Mariotte's law), if the pressure changes - provided the nostrils or mouth are open and in communication with the outside world - the volume must now increase isobarically (i.e. at the same pressure). The lung fills up, inspiration is finished.
In diaphragmatic breathing, the diaphragm lowers only by contraction (the diaphragm is made of muscle), causing the lungs to stretch downward.
Expiration usually takes place passively, because after inspiration the lungs and thorax are stretched to such an extent that elastic deformation work is stored in them (similar to a spring that is first tensioned and then released), which expels the "used" air from the lungs. If expiration takes place with the participation of the expiratory respiratory muscles, it is called forced expiration. The intercostal muscles contract first, but various other respiratory muscles may also be involved. The latissimus dorsi muscle ("cough muscle") plays a special role in connection with forced expiration.
See also: Lung volume and lung function
Diseases
See also: Pneumology and List of diseases of the respiratory system according to ICD-10
Pulmonary embolism. In pulmonary embolism, an embolus blocks one of the blood vessels (vein) that supplies blood to the lungs, causing a section of the lung to no longer be supplied with blood. This disease can be compared to a heart attack.
Obstructive pulmonary disease. In chronic obstructive pulmonary disease (COPD), a narrowing of the airways obstructs the flow of air. This often leads to shortness of breath (dyspnoea). The most important risk factor is smoking, but environmental pollution, low birth weight and genetic factors are also thought to be responsible. COPD includes chronic bronchitis and emphysema. Pulmonary emphysema can also develop from a hereditary metabolic disorder called alpha-1 antitrypsin deficiency.
Restrictive lung disease. In contrast, in restrictive lung disease, the flexibility of the lungs is restricted (in the sense of: restriction of lung mobility). This reduces lung volume and compliance, that is, distensibility relative to pressure. These include sarcoidosis, pneumoconiosis (pneumoconiosis) and other diseases that result in fibrosis of the lung tissue, but also external influences such as deformities of the thorax (kyphosis, scoliosis).
Pulmonary edema. Pulmonary edema refers to the accumulation of fluid in the lung tissue. A distinction is made between permeability edema (ARDS, toxic pulmonary edema), in which the permeability of the capillaries is increased, and hydrostatic pulmonary edema (cardiac edema, high-altitude edema), in which the pressure in the capillaries exceeds the pressure in the alveoli to such an extent that the fluid is "forced" out of the capillaries.
Atelectasis. In atelectasis, a section of the lung has collapsed and the alveoli contain no or very little air.
Pneumothorax. If the pleural space gains access to air from the inside or outside, the negative pressure in the pleural space collapses and the corresponding lung collapses. Unlike a completely absent lung, a pneumothorax means a functional right-to-left shunt, since blood from the systemic circulation re-enters the systemic circulation via the affected lung without substantial oxygenation, so that full saturation cannot be achieved.
Tuberculosis. Tuberculosis, an infectious disease whose causative agent is Mycobacterium tuberculosis, is transmitted by droplet infection and manifests itself first in the lungs. X-rays show characteristic moth-eaten lesions, which also gave the disease the nickname "the moths".
Inflammations. Inflammations in the lungs are divided into pneumonias (lung inflammations), in which the lung tissue is affected, bronchitis as inflammation of the bronchi and bronchiolitis, the inflammation of the small bronchi.
Neoplasms. Cancers of the lungs are called bronchial carcinoma because they are malignant neoplasms of degenerated cells of the bronchi or bronchioles. It is one of the most common malignancies in humans. According to the World Health Organization, different subtypes are distinguished on the basis of histology: squamous cell carcinoma, adenocarcinoma, small and large cell carcinoma and other rare types. In addition, metastases of other tumors are often found in the lungs due to their filtering function.
In the event of respiratory arrest, the lungs can be ventilated - pulsatingly - by filling them with a small amount of excess air pressure via the bronchi, which serves to maintain life in an emergency or during anaesthesia.
Human lungs
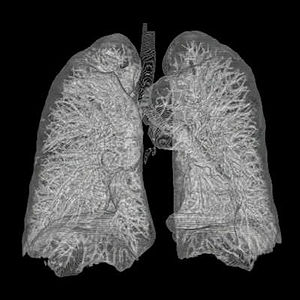
3D reconstruction of human lungs from CT images
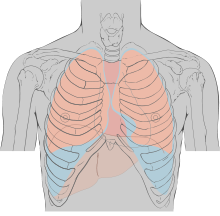
Expansion of the lungs during inhalation (blue) and exhalation (pink)
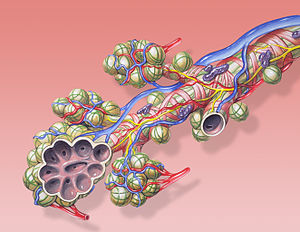
Structure of a terminal bronchiolus (last alveolar bronchial branch).
Questions and Answers
Q: What is the function of the lung in vertebrates?
A: The lung takes blood oxygen from the air and expels carbon dioxide.
Q: How many lungs do most vertebrates have?
A: Most vertebrates with lungs have two of them.
Q: What happens in the lungs during gas exchange?
A: The lungs are the area where gas exchange takes place. Without gas exchange, oxygen would not pass into the blood from the lungs so the body cells would not be able to receive the oxygen needed for respiration.
Q: What are alveoli?
A: Alveoli are moist structures in the lungs that allow oxygen to move from the lung through the alveoli into blood vessels and red blood cells.
Q: What is the function of carbon dioxide in the lungs?
A: Carbon dioxide passes from the blood into the alveoli.
Q: Where does oxygen-filled blood go after leaving the lungs?
A: The oxygen-filled blood goes back to the heart.
Q: Where does carbon dioxide go after leaving the lungs?
A: The carbon dioxide in the alveoli is pushed out of the lungs and into the air we breathe out.
Search within the encyclopedia