Diabetes
![]()
This article is about human diseases. For diabetes mellitus of the dog, see Canine diabetes mellitus. For diabetes mellitus of the cat, see Feline diabetes mellitus.
Diabetes mellitus ('honey-sweet flow', 'honey urine dysentery'; from ancient Greek διαβήτης diabḗtes [to διαβαίνειν diabainein, German 'to pass through', 'to flow through'] and Latin mellitus 'honey-sweet'), colloquially diabetes for short, German Zuckerkrankheit (formerly also Zuckerharnruhr) or, more rarely, Blutzuckerkrankheit, refers to a group of metabolic disorders of carbohydrates based on an (absolute or relative) deficiency of insulin, leading to chronic hyperglycaemia. The hallmarks of this complex disorder include hyperglycemia, glucosuria, acidosis, and ketosis.
The word describes their main symptom, the excessive excretion of sugar in the urine. Thomas Willis diagnosed the disease in 1675, as did ancient doctors in India, Alexandria and Rome, on the basis of a taste sample of urine, because the urine of people with diabetes has a sweetish taste when blood sugar levels are elevated.
Mechanisms that lead to hyperglycaemia predominantly affect insulin, the main regulatory hormone of sugar metabolism in the human body: absolute insulin deficiency, relative insulin deficiency due to weakened effectiveness of insulin (insulin resistance) or both together. Consequences of diabetes mellitus are mainly changes in the nervous system and the vascular system, including diabetic foot syndrome.
For the history of diabetology, and in particular the history of insulin as an active ingredient, see History of diabetology.
Physiological basics
→ Main article: Insulin, glycogen and gluconeogenesis
The digestive system breaks down the carbohydrates ingested with food (from fruits, cereal products, potatoes, corn, rice) into glucose (dextrose), which is then absorbed through the intestinal wall into the blood and distributed throughout the body.
The pancreas produces the hormone insulin in the β-cells of the islets of Langerhans. As a messenger substance, insulin causes the transport of glucose into the cell interior, where the glucose is subsequently consumed for energy production (glycolysis). In addition, insulin also causes glucose to be stored in the form of glycogen in the liver as well as in the muscle cells, which keeps the blood glucose level constant within narrow limits (approx. 80-120 mg/dl or 4.5-6.7 mmol/l) after food intake.
Even during long periods of fasting, the blood sugar level remains at a normal level, which in turn is mainly ensured by the liver, on the one hand by the previously formed glycogen being split back into glucose and released back into the blood, and on the other hand by the liver constantly producing new glucose biochemically (gluconeogenesis).
If the insulin-producing β-cells no longer produce enough insulin or no insulin at all, or are no longer present at all, e.g. due to inflammation or surgery, both glucose uptake into the body's cells and the inhibition of new glucose formation in the liver (which can produce up to 500 grams of new glucose per day in humans) are therefore missing. This new formation explains the rise in blood glucose levels in diabetics, e.g. in the early morning when they are fasting (see also Dawn phenomenon).
In diabetes mellitus, the ingested glucose remains in the blood, or the body's own new glucose formation in the liver continues unchecked and constantly supplies glucose, which balances or even exceeds the continuous consumption and as a result causes the blood sugar to rise. It is a very complex and dynamic biochemical process in which inflows, outflows, new formation and degradation of glucose must be constantly balanced, i.e. accounted for. In order to understand these interrelationships - and thus the disease and how to deal with it - affected patients must be carefully informed and advised and, if necessary, trained, for example in the preparation of suitable dietary plans.
In addition, insulin has another, third effect. It is the only hormone in the human body that builds up body fat and also ensures that this fat remains in the depots (so-called adipogenic effect).
A major characteristic of severe, persistent insulin deficiency is therefore also extreme weight loss due to the elimination of the adipogenic effect, in particular the breakdown of body fat and (muscle) protein for energy production.
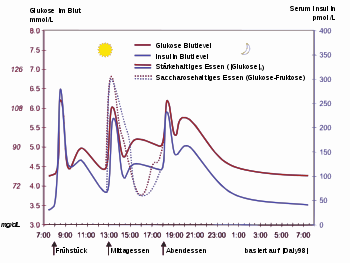
The picture shows the regulation of blood glucose (red) and the blood glucose controlling hormone insulin (blue) in a healthy person over the course of the day with three meals. Also shown is the influence of a sugary (dashed) versus a starchy (solid) meal.
Classification of diabetes mellitus into types
In 1965, the World Health Organization (WHO) published a distinction between different types of diabetes in its "Recommendations on Classification and Diagnosis".
In 1997, the American Diabetes Association (ADA) changed the criteria for classification and diagnosis, which were adopted by the WHO in 1998 and by the German Diabetes Association (DDG) in 2000. In the model, a distinction was no longer made between insulin-dependent diabetes mellitus (IDDM) and non-insulin-dependent diabetes mellitus (NIDDM), as this classification only refers to treatment and not to the cause of the disease. Since 2009, the definition no longer distinguishes between subgroups a and b. The ranking of diabetes types from A-H was also abandoned.
Classification until 1997
Until that date, diabetes mellitus was divided into four groups according to the type of treatment, the fifth designated that the disease is not present:
- NIR: (non-insulin-requiring) treatment without external insulin supply, e.g. with diet and/or oral antidiabetics only.
- IRC: (insulin requiring for control) In addition to the body's own insulin, external insulin is also required to lower elevated blood glucose levels.
- IRS: (insulin requiring for survival) External insulin supply is required for survival. According to the new classification, these are type 1 diabetes and type 2 diabetes with severely reduced or discontinued own insulin production.
- IGT: (impaired glucose tolerance) Impaired glucose tolerance.
- ND: (non diabetic) Not suffering from diabetes.
Diabetes types since 1998
Since that date, all organizations divided the disease into the following four types according to the cause:
- Diabetes mellitus type 1: T-cell mediated autoimmune disease with destruction especially of the beta cells of the islets of Langerhans in the pancreas, usually leading to absolute insulin deficiency.
- Diabetes mellitus type 2: Different combinations of insulin resistance, hyperinsulinism, relative insulin deficiency, secretion disorders
- Type 2a: without obesity (adiposity)
- Type 2b: with obesity
- Other specific types of diabetes
- A: genetic defects of the beta cells of the islets of Langerhans (impaired insulin secretion)
- B: rare genetic defects of insulin action
- C: Pancreas diseased or destroyed
- D: Diabetes due to hormonal disorders (endocrinopathies)
- E: Diabetes caused by medications or chemicals (drugs, toxins).
- F: Diabetes mellitus due to infections
- G: unusual forms of immune-mediated diabetes
- H: other genetic syndromes associated with diabetes
- Gestational diabetes (pregnancy diabetes)
Diabetes types according to the DDG 2009 guidelines
Based on the report of the WHO Commission of 1999, the following criteria are used for classification according to the guidelines of the DDG 2009:
- Type 1 diabetes mellitus: Destruction of the beta cells of the pancreatic islets of Langerhans leads to absolute insulin deficiency.
- Type 2 diabetes mellitus: Can range from (genetic) insulin resistance with relative insulin deficiency to absolute insulin deficiency later in the course of the disease. It is often associated with other metabolic syndrome problems.
- Other specific types of diabetes
- Diseases of the exocrine pancreas (e.g. pancreatitis, cystic fibrosis, haemochromatosis)
- Endocrinopathies (e.g. Cushing's syndrome, acromegaly, pheochromocytoma)
- Drug-chemically induced (e.g. glucocorticoids, neuroleptics, alpha-interferon, pentamidine)
- Genetic defects of β-cell function (e.g. MODY forms)
- Genetic defects of insulin action
- Other genetic syndromes that may be associated with diabetes
- Rare forms of autoimmune-mediated diabetes.
- Gestational diabetes: glucose tolerance disorder first encountered or diagnosed during pregnancy. This includes:
· Initial manifestation of type 1 diabetes
· Initial manifestation of type 2 diabetes
· Initial manifestation of other specific types of diabetes
· Preconceptionally manifest but undiagnosed diabetes mellitus (type 2), especially to be assumed in the case of glucose tolerance disorders already in the 1st trimester.
This classification was confirmed by the DDG in 2011 as part of an update of the guidelines.
Other terms
- Juvenile diabetes mellitus or "juvenile diabetes mellitus" is the outdated term for type 1 diabetes.
- Adult-onset diabetes mellitus or "adult-onset diabetes" used to be the name given to type 2 diabetes. Both terms are still widely used, but do not reflect the current state of science and are therefore no longer included in the current classifications.
- LADA: Type 1 diabetes mellitus also includes LADA (latent autoimmune diabetes with onset in adults). This form concerns the autoimmune diabetes that develops in older adults, which after a relatively short time no longer responds to oral medication and becomes insulin-dependent. Typical is the detection of the GAD (=glutamate decarboxylase) antibody.
- MODY: MODY (maturity onset diabetes of the young) corresponds to the progression form of type 2 diabetes, but without the occurrence of obesity and insulin resistance, instead it already occurs in children and adolescents.
- IDDM: Abbreviation for insulin dependent diabetes mellitus. Outdated, but still widespread classification according to the necessary form of therapy.
- NIDDM: Abbreviation for non insulin dependent diabetes mellitus. Outdated, but still widespread classification according to the necessary form of therapy.
Questions and Answers
Q: What is diabetes insipidus?
A: Diabetes insipidus is a disease that is unrelated to diabetes mellitus.
Q: What do people usually mean when they say "diabetes"?
A: When people say "diabetes", they usually mean diabetes mellitus.
Q: What are diabetics called?
A: People with diabetes Mellitus are called "diabetics".
Q: What is glucose?
A: Glucose is a natural carbohydrate that our bodies use as a source of energy. It is different from the kind of sugar sold in supermarkets, which is called sucrose. High concentrations of glucose can be found in soft drinks and fruits.
Q: How does the body control the glucose level in the blood?
A: The glucose level in the blood is controlled by several hormones. Hormones are chemicals in the body that send messages from cells to other cells. Insulin, which is made by the pancreas, sends a message to other cells in the body when you eat telling them to take up glucose from the blood for energy or store it as glycogen for later use.
Q: How does insulin work?
A: Insulin tells cells to take up glucose from the blood and use it for energy or store it as glycogen for later use when you eat. When you are not eating, cells break down stored glycogen into glucose to use as energy.
Q: Where can high concentrations of glucose be found?
A: High concentrations of glucose can be found in soft drinks and fruits.
Search within the encyclopedia