COVID-19 pandemic
![]()
This article describes a current event. The information may therefore change rapidly.
The COVID-19 pandemic (pronunciation: [koːvɪtˈnɔɪ̯ntseːn], also Corona(virus) pandemic or Corona(virus) crisis) is the worldwide outbreak of the respiratory disease COVID-19 (predominantly called "Corona" in German-speaking countries). The pandemic has dramatic effects in many countries.
On December 31, 2019, an outbreak of a new pneumonia with an as yet unknown cause was confirmed in Wuhan, China. On February 11, 2020, the World Health Organization (WHO) proposed the name COVID-19 for the infectious disease. In January 2020, the disease became an epidemic in China, and on March 11, 2020, WHO officially declared the previous epidemic a global pandemic. The disease is caused by an infection with the previously unknown coronavirus SARS-CoV-2. In numerous countries around the world, there are massive cuts in everyday life in the course of the pandemic. The overall social impact of the COVID-19 pandemic also includes the economic crisis of 2020/21.
The third and so far most devastating pandemic of the 21st century is being widely covered by the media worldwide. It is an example of the rapid spread of a disease in an interconnected and globalized world.
On January 13, 2020, the first laboratory test-confirmed Corona infection outside of China occurred in Thailand, and the first outside of Asia occurred in the United States on January 23, 2020. In both cases, there was an association with travel to or from Wuhan. To counter the spread to countries without effective health systems, WHO declared the coronavirus pandemic a "public health emergency of international concern" on January 30, 2020.
The first Corona-related death outside China was registered in the Philippines in early February 2020; it was a Chinese man from Wuhan. On February 9, 2020, the number of registered deaths already exceeded the total number of deaths from the 2002/2003 SARS pandemic, exceeding 800. On February 15, 2020, an eighty-year-old Chinese man died in France as a result of Corona infection. The Chinese tourist was the first fatality of the COVID-19 pandemic in France and the first outside Asia.
On February 23, 2020, the first two Europeans became victims of the COVID-19 pandemic in Italy. As of February 28, 2020, the WHO assessed the risk at the global level as "very high" in its reports (English WHO risk assessment, global level: very high), previously as "high".
On March 19, 2020, Italy reported more deaths than China for the first time. By mid-March 2020, most cases of infection were in China, Italy, Spain, Iran, Germany, France, and the United States; few new infections were reported from China. At the end of March 2020, the number of corona infections in the United States rose sharply; thus, the United States also became a focal point ("hotspot") of the global COVID-19 pandemic, along with Europe and China.
In May and June 2020, Latin America emerged as the new center of the coronavirus pandemic, with Brazil, Peru, Chile, Mexico, Colombia, Argentina, Ecuador, and Bolivia particularly affected.
At the end of August 2020, India reported the highest number of new infections in one day worldwide for the first time. India thus became the new center of the pandemic.
In September 2020, a sharp increase in cases was recorded in Europe, which has continued steadily. It was dubbed the "second wave". In the USA, on the other hand, the start of the "third wave" occurred shortly thereafter. Both waves were described as significantly more aggressive.
As of September 29, 2020, WHO reported over 1,000,000 confirmed COVID deaths out of over 33,000,000 confirmed infected persons. However, these are only the confirmed case numbers, not including the number of unreported cases. Excess mortality calculations by the Economist, a British business magazine, found that by August 2020, approximately 1.5 to 2 million people (0.019-0.026% of the world's population) had died as a result of COVID-19 and 500 to 730 million had become infected. The cumulative calculated number of infected people reaches 6.34-9.3% of the world population. However, the excess mortality data are limited to Western European countries, some Latin American countries, Russia, the United States, South Africa, and several other major countries. A further calculation of the true extent of the pandemic, to be conducted by WHO, is being planned. As of May 2021, WHO estimated that approximately 6-8 million people have died from COVID-19 to date.
In December 2020, the virus variant VOC-202012/01 (B117) was reported in the United Kingdom to be 70 percent more contagious than the previously predominant virus type. In South Africa, the virus mutation 501.V2 is spreading, in Brazil the variant Lineage P.1 and in India the variant B.1.617.
On January 28, 2021, the number of confirmed infections worldwide surpassed 100 million.
Disease
→ Main article: COVID-19
See also: SARS-CoV-2 #Discovery History
The COVID-19 disease and the SARS-CoV-2 pathogen that triggered the epidemic at the end of 2019 were not previously known. Therefore, in the course of what was initially classified as a local outbreak and relatively quickly became an epidemic, essential knowledge about the disease first had to be gained. This involved the disease-causing trigger as well as basic metrics that determine the dangerousness of a disease and the facts surrounding its spread and possible measures against it. At the same time, the rapid spatial spread and other characteristics of the disease made it difficult to collect sufficiently accurate data to determine the spread, extent, and hazard with scientific precision (see the Statistical Estimates and Simulation Studies section below).
Initially, local authorities did not assume human-to-human transmission, direct infection, because this is the exception for a pathogen that passes from animals to humans, a zoonotic disease, and they thought they had not initially identified any such cases. After the pathogen was identified as a novel subspecies of the viral species Severe acute respiratory syndrome-related coronavirus (SARSr-CoV for short), disease fighters assumed conditions similar to those of the previously known disease Severe acute respiratory syndrome, triggered by the virus previously known as SARS-CoV and later often referred to as SARS-CoV-1 to distinguish it from the newly discovered virus, and the SARS pandemic of 2002/2003 triggered by it. As it later turned out, these assumptions were wrong, especially regarding human-to-human transmission and spread of the disease by carriers with no or only very mild symptoms.
During February 2020, it became apparent that COVID-19 is transmitted much more readily than SARS, that many infected people have no symptoms, and that asymptomatically infected people or infected people with no clear symptoms or no symptoms yet can be contagious. Cases have been reported of people infecting other family members without showing symptoms themselves. When it was still not entirely clear in mid-March 2020 exactly what role these silent carriers were playing in the pandemic, data from the Chinese government suggested that about one-third of those who tested positive were probably asymptomatic and were causing a relevant proportion of the infections. In addition, during the first weeks of the epidemic, the authorities in Wuhan were overwhelmed, leading to such a high number of unreported cases in that region "that the cases counted there are not very meaningful," says epidemiologist René Niehus.
The World Health Organization noted in a July 9, 2020, publication that the virus can also be transmitted by aerosols and that infected individuals can act as carriers both with and without symptoms.
Dangerousness of the disease
Different factors are considered to assess the danger posed by an epi- or pandemic: A distinction must be made as to whether a disease poses a threat individually to a specific person, to a specific population group, to the population of a state, to a region, or to the entire world. In its daily reports, WHO therefore designated the hazard situation separately for China, Regional Level and Global Level (as of February 26, 2020). The most important characteristics of an epidemic are the transmission rate, the spread dynamics (temporally and spatially), the proportion of severe courses, the lethality, and the incubation period. Some of these data can only be determined retrospectively, see the section Problems of interpretation in the article Lethality. Others are largely determined by human behavior and are therefore highly variable. This is particularly true for spatial spread and baseline reproduction numbers, which are strongly influenced by individual factors such as travel behavior, modes of communication and contact, and hygiene behavior.
On February 19, 2020, WHO summarized the scientifically validated findings to date (based in part on estimates from model calculations):
- Time between infection and onset of symptoms (incubation period): 0-14 days (median 5-6 days).
- Time between "case 1" and the "case 2" infected by it in a transmission chain (serial interval): around 5-7 days
- Lethality: was not known with certainty. The WHO distinguishes between two forms of calculation. One is the ratio of the number of cases of a given disease with fatal outcome in a given period to the number of confirmed cases in the same period, the confirmed case fatality ratio. The other is the proportion of deaths among all infected persons, the IFR for infection fatality ratio. For both variants, only limited reliable statements are possible during a dynamically spreading wave of disease with presumably high numbers of unreported cases. The statistical probability that an infected person will die regardless of individual characteristics, the IFR, is given by WHO as 0.3-1%; a February 2020 paper cited by WHO gives a preliminary estimate of 0.4-2.6%, with the most likely value given as 0.94%.
Other basic findings (compare main article on the disease) were:
- Severe courses of the disease, especially those in which the lungs are affected, often result in long-term damage. In addition to damage to the lungs, damage to the heart muscle is also known. Even supposedly harmless courses of the disease can cause very pronounced changes in the lungs, of which - as of March 2020 - it is not known whether they will regress.
- The number of people infected by one infected person (baseline reproduction number) was 3.28 (arithmetic mean) and 2.79 (median), or about three people, by February 7, 2020, according to a metastudy of 12 papers.
- Differences between different populations exist, especially in cases with severe complications and fatal outcome, although all can be infected.
- Transmission occurs via droplet infection, for example also through aerosols - a subtype of droplet infection. It has not been proven that transmission also occurs by touching contaminated surfaces and objects (smear infection); however, officials warn against this.
- At the end of February 2020, the question of virulence, i.e. the proportion of people with (severe) symptoms in the total number of infected people, was highly uncertain. To this end, as the WHO Report - 29 cited above indicates, there is a lack of serial surveys to determine the true proportion of infected people in the population. In particular, however, the clusters studied in non-Chinese foreign countries indicate an overall low virulence compared to SARS.
- Equally uncertain is the infectivity, i.e. how likely infection is in the event of exposure to the virus. This infectivity is only partly determined by the virus itself (its contagiosity), but also by how healthy the exposed person is, how well his or her immune system responds to the virus, and by how many viruses the person is exposed to and for how long. Rough estimates suggest a much higher infectivity than SARS, but smaller than measles, for example.
In mid-February, a Chinese study was published that examined 44,672 confirmed COVID-19 cases. Eighty-one percent of patients had mild forms of COVID-19, and in about 14 percent of cases, the virus caused severe disease progression with pneumonia and dyspnea. About five percent of patients experienced respiratory failure, septic shock, or multiple organ failure. In about two percent of cases, the disease was fatal. According to the study, the risk of dying increases with age. According to the WHO, there are relatively few cases of children with the disease. In a mild course of the disease (the most common case), the signs of illness, if any, usually resolve within two weeks, according to the WHO. People with a severe course of the disease take between three and six weeks to recover from it.
Risk groups
Different proportions of the population had particular risks for infection, disease, or severe disease progression.
According to WHO, 95% of all deaths reported in Europe in April 2020 were in the over-60 age group. More than 50% of these deceased were over 80 years old. In Moscow and in some Swiss cantons, measures specifically tailored to seniors have been ordered. A March 17, 2020, survey of decedents with positive COVID-19 in Italy found that only 0.8% of these individuals had no preexisting disease, while 25.1% had one preexisting disease and 25.6% had two. Three or more preexisting conditions were found in 48.5% of cases.
Comparison with influenza (flu)
See also: COVID-19 #Estimation of mortality risk.
The study by Mike Famulare of the Institute for Disease Modeling, cited by WHO, designed a scale for the transmissibility and clinical severity of COVID-19 using a framework for assessing influenza epidemics and pandemics. According to this, COVID-19 is as easily transmissible as Spanish flu, but one level lower in clinical severity, and thus overall one level less severe than the latter, but two levels more severe than Asian flu and Hong Kong flu. It is now also thought to be potentially equivalent to Spanish flu in clinical severity. A blanket comparison between COVID-19 and influenza is not possible because the influenza virus is extremely mutable and each flu wave, each flu season differs significantly in its basic levels. COVID-19 has become endemic. The novel coronavirus has been shown to mutate, giving rise to variants of SARS-CoV-2.
In February 2020, Alexander S. Kekulé, a virologist at Halle University Hospital and director of the Institute of Medical Microbiology, compared the "dangerousness" of the COVID-19 pandemic to the consequences of influenza in the past:
"Of course, it's the case that in some seasons in Germany, the flu causes several thousand - there was even a case once where it caused over 20,000 deaths. Yes, the flu does that, but you always have to put that in perspective. Of course, we also had over ten million infected people in Germany in the year when it was so high. If you then break that down, the mortality of the flu is 0.1 percent or one in 1,000, and at most one in 1,000, and the mortality of this coronavirus is 0.5 to 1.5 percent, somewhere in the range, that is, I'll say roughly one in 100. That means the virus is ten times more dangerous for the person who gets the infection."
- Alexander Kekulé in an interview in February 2020: deutschlandfunk.de
Lothar H. Wieler, head of the Robert Koch Institute (RKI), made a similar statement on February 27, 2020. Here, he compared the percentages of deaths among infected persons during a mild flu season (lethality of 0.1-0.2%) with an assumed lethality of 1-2% during the SARS-CoV-2 epidemic. Michael Spitzbart, Wolfgang Wodarg, and Sucharit Bhakdi suggested in March 2020 that COVID-19 was no worse than previous influenza waves. Virologist Jonas Schmidt-Chanasit rated the situation on COVID-19 as more of a concern in principle in late February 2020, but compared it to influenza at the time, concluded that COVID-19 was still far from the level of seasonal influenza, with about 650,000 deaths worldwide per year, although that could change soon. He pointed to the lack of population immunity for COVID-19 as opposed to normal seasonal influenza, as well as a lack of vaccination options.
Recovery and immunity
Since the virus first spread to humans as a zoonosis, the population had no adaptive immunity, i.e., no immunity acquired through previous contact with the pathogen or vaccination. Cross-immunity due to very similar pathogens already circulating is also not known or likely to exist. Herd immunity is mainly important for the development of an epidemic in the general population. For COVID-19, the population proportion of people who have become immune in which herd immunity occurs was estimated to be about 60% to 70% in March 2020. However, according to immunologist Michael Meyer-Hermann, achieving this through contagion is not possible in the foreseeable future in April 2020 without collapsing the healthcare system.
How long immunity from natural infection lasts was also unknown, according to a 2020 WHO statement.
See also: herd immunity #debate about herd immunity through natural contagion.
There was debate about whether herd immunity should be achieved naturally or through a vaccine. However, the strategy of relying on natural herd immunity was called unethical and scientifically problematic by the WHO in 2020.
· Test on COVID-19
· 
Temperature measurement
· 
Swab from a nose ...
· 
... and in the throat
· 
Samples are packed for transport to the laboratory
Prevention
→ Main article: COVID-19 #Prevention
The aim of social prevention is to stop or slow down the spread of a disease as far as possible. In addition to the characteristics of the virus (see section Dangerousness of the disease), the spread of an epidemic is largely characterized by people's social behavior. Therefore, hygiene measures, early detection and the management of contacts (identification and, for example, domestic isolation or quarantine) are the first measures to prevent or slow down the further spread of the virus.
In the event of further spread, a wide variety of measures are taken, all of which are aimed at social distancing, i.e. increasing the social distance, reducing contact and physical distance. The reason for this is that social proximity (number and type of meetings, manners, and physical distance) is a major determinant of the baseline reproduction number for pathogens transmitted from person to person, i.e., the number that indicates how many people an infectious person infects on average. When a pathogen becomes endemic and it is thus no longer considered containable and eradicable, the precautionary goals change from "control the spread" to "slow the spread and provide health care." The overriding goal in this phase is "to avoid the simultaneous illness of extremely large numbers of people requiring treatment and the resulting threat of overloading the medical infrastructure".
· 
No visiting sign in the Munich Bogenhausen Clinic
· 
Distance control in a theater in Kavala, Greece
· 
Urinals blocked due to the distance regulation
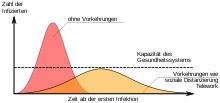
Simplified model for the "flattening of the pandemic wave" if no vaccinations are carried out: without protective measures, rapid increase in the number of ill people and overloading of the healthcare system (red); with protective measures, slower spread, fewer people ill at the same time, so that all patients can be cared for (yellow)
Origin and course of the pandemic
Origin
→ Main article: SARS-CoV-2 #Origin and host range.
The causative virus probably originates from the animal kingdom, although the pathogen reservoir is not yet completely clear. Initially, it was assumed that the virus originated from bats, from which it passed to humans via an intermediate host, probably another mammal (zoonosis).
Deforestation of rainforests, global warming, and wildlife trafficking are considered factors that promote the spread of diseases.
In late March 2020, it was suspected that the virus was just as likely to have originated from the pangolin. It was also suspected that recombination had occurred in a double infection and that the SARS-CoV-2 virus was a new chimera created from a virus similar to the virus isolated from bats and a virus similar to the virus isolated from pangolins.
The first known cases of COVID were in November and December 2019. Because several of those first infected worked as vendors or traders at the "South China Wholesale Fish and Seafood Market Wuhan" (Chinese 武汉华南海鲜批发市场, pinyin Wǔhàn huánán hǎixiān pīfā shìchǎng), this was suspected to be the primary site of infection. In addition to marine animals, many other wild animals used in Chinese cuisine and traditional Chinese medicine were also traded on the wet market. It was later revealed after a study by Wuhan Hospital that the first identified patient had not been at this market. On Dec. 31, 2019, the China National Health Administration sent a team to Wuhan to investigate the unclear cases. Authorities and WHO initially incorrectly assumed that the agent causing the infection was not transmissible from person to person or was very difficult to transmit.
Research on the timing and location of the outbreak is ongoing:
- On December 31, 2019, the HealthMap medical information system and BlueDot, a Canadian company in the United States, informed WHO and CDC of a striking increase in reports of pneumonia (pneumonia) of unclear etiology in the Wuhan region.
- An article in the journal Science summarized the research results of several groups on genetic mutation and origin in late January 2020. According to the article, several groups estimated the start of spread to be mid-November 2019, and one group even estimated September 18, 2019.
- According to a March 2020 South China Morning Post report, government records show that the first patient whose samples were subsequently attributed to COVID-19 may have become infected on November 17, 2019. From that date, between one and five cases had been recorded daily. None of the early cases are considered "patient zero." By Dec. 15, 27 people had been infected, according to the report, and double-digit new infections occurred for the first time on Dec. 17. By Dec. 27, more than 180 people had been infected, and by year's end, at least 266 people had been infected, it said. At the beginning of the year, there had been 381 infections without these cases, which were unclear at the time, being released to the public.
- A May 8, 2020, Süddeutsche Zeitung article reports research results that use phylogenetic analysis to narrow the outbreak to between September 13 and December 7, 2019, with a 95% probability. The article cites the Chinese provinces of Yunnan and Guangdong as possible locations of the outbreak.
- On August 3, 2020, WHO Executive Director Michael Ryan stated that significant clarification is still needed on the questions of the origin and initial spread of the SARS-CoV-2 virus. Although Wuhan was the first place where the new pneumonia was officially detected, other places in China could also be considered as the initial site of spread.
- According to a dermatology study from Italy, the virus was detected in the skin sample of a 25-year-old woman from Milan as early as November 10, 2019. An even earlier occurrence in Italy is indicated by a cancer study, according to which SARS-CoV-2 antibodies were found in blood samples as early as September 2019.
Worldwide expansion in the early days
See also: COVID-19 pandemic #statistics and modeling of the epidemic.
Asia
People's Republic of China
→ Main article: COVID-19 pandemic in the People's Republic of China.
In the summer of 2020, researchers at Harvard Medical School presented a study in which they used satellite photos of the parking lots outside six hospitals in Wuhan to track traffic volumes. They located an increase in traffic in September and October 2019 and speculated that the virus had already begun to spread during that period. Critics objected to the study's methodology as cherry-picking.
December 2019
The local health authority was informed of the finding of a SARS-like pathogen no later than December 27. China had introduced an early warning system after the experience of the SARS pandemic to ensure that disease information was immediately forwarded to the Chinese Center for Disease Control and Prevention, regardless of political considerations. However, this did not happen in the case of the novel coronavirus.
On December 30, Chinese physician Li Wenliang warned of a viral outbreak within a WeChat group with colleagues in light of an unusual cluster of pneumonias (lung infections) at a local hospital in Wuhan. At that time, he assumed that it was the causative agent of severe acute respiratory syndrome (SARS). After Li and his colleagues' warning went viral on the Internet, he and at least seven other of his colleagues were summoned by local police. They were accused of "making untrue allegations" that "seriously disturbed social order" and were required to sign confidentiality agreements under threat of harsh penalties, though Li Wenliang later violated them. On Jan. 1, 2020, the state-run Xinhua news agency reported the doctors' alleged "false reports" and reiterated that there was no evidence of human-to-human transmission of the new disease. Li Wenliang died Feb. 7, 2020, at age 33, presumed dead of the disease he had previously warned about. The doctors, on their own initiative, had continued to bypass official channels and send patient samples to analytical laboratories to investigate the cause of the disease on their own. They were rehabilitated by the Supreme People's Court at the end of January.
The Chinese government is accused of actively concealing the outbreak of the disease and thus enabling its unhindered spread in the first place. Although the new virus had already been discovered and sequenced in December 2019, the ChineseCommunist Party ordered the research institutions to stop the tests and destroy the samples in January and imposed a press ban.
On December 31, 2019, Chinese authorities officially informed the World Health Organization (WHO) that several cases of severe pneumonia had occurred in the city of Wuhan since early December 2019, the causative agent of which had not yet been identified and was believed to be caused by an as-yet uncharacterized pathogen. The announcement was disseminated through news agencies the same day. The U.S. Centers for Disease Control (CDC) then also learned of the pneumonia cluster in Wuhan. A CDC epidemiologist who had previously worked embedded with the Chinese health authority and whose job would have included sharing early information about potentially dangerous outbreaks had been recalled by the U.S. government in July and the position had not been filled.
Between December 31, 2019 and January 3, 2020, a total of 44 cases of pneumonia with unknown cause were reported to WHO from Wuhan.
Year 2020
The fish market in Wuhan was closed and disinfected by local authorities on January 1, 2020. On January 5, 2020, the Chinese Center for Disease Control and Prevention ruled out MERS-CoV and SARS-CoV as the causative agent based on test results. On January 7, 2020, the Chinese side announced the identification of a novel coronavirus in several ill persons. The virus was given the provisional name 2019-nCoV (2019 novel coronavirus). On January 13, 2020, the Ministry of Health of Thailand announced that the novel virus had been detected in Thailand, in a traveler from Wuhan. On January 15, an analogous case was reported from Japan, and on January 20, a case was reported from South Korea.
Based on the fact that cases of the disease had occurred in several long-distance travelers, epidemiologists concluded that the number of cases of the disease must be far greater than the 44 cases initially reported. Experts estimated on January 17, 2020, that the number of people infected in Wuhan was about 1,700, and the fact that several members of the hospital staff involved in treating the sick people also became ill made it clear that human-to-human transmission was possible. This was confirmed by the Chinese authorities on January 20, 2020.
As recently as January 18, nearly 40,000 families in Wuhan gathered unhindered for Chinese New Year (potluck) celebrations. It is suspected that this resulted in a particularly large number of infections.
Meanwhile, the disease had also reached Beijing, where infected people had been concentrated in certain hospitals since January 20.
Up to and including January 26, 2020, official Chinese data indicated that 2,744 infected persons had been registered in China. The number of confirmed fatalities rose to 80 (all in China). On January 26, 2020, Hubei province, including the city of Wuhan, was classified by the German Robert Koch Institute as the first risk area in China.
On January 27, 2020, Chinese state television reported an increase of 1,200 illnesses, bringing the total number of cases reported in China to about 4,000; a discrepancy of 500 from WHO figures.
In early February, the number of new infections in China initially appeared to be declining. On February 7, 2020, the German Robert Koch Institute declared that Chinese risk areas would be expanded to include four major cities (Wenzhou, Hangzhou, Ningbo, and Taizhou) in Zhejiang province near the coast in eastern China in the previous risk area. On Feb. 13, Chinese authorities changed the reporting criteria and, in a departure from WHO guidance, clinically diagnosed cases without virus detection were also included. This resulted in the highest number of new cases reported for Hubei alone, 14,000. This change was reversed on February 20, and the reporting criteria have since returned to WHO specifications. On February 14, 2020, the National Health Commission announced that 1716 health care workers were infected as of the reporting date. Six of these were reported as deceased. As of February 20, 2020, there were 2,055 laboratory-confirmed infections among healthcare workers, 88% of them in Hubei Province, in a total of 476 Chinese clinics.
On February 18, 2020, the number of new infections per day in China was below 2,000; on February 20, it dropped below 1,000; and according to the WHO report of February 26, 2020, for the first time, there were more new infections outside China (460) than inside (410). The joint mission (WHO-China joint mission in English) conducted by WHO with China from February 16 to 24, 2020, concluded that the radical measures implemented in China were suitable to contain the virus and significantly reduce the number of newly infected people since the end of February 2020. This was achieved through intensive follow-up of infected individuals and their contacts. Restrictions on human-to-human transmission by canceling numerous major events and extending vacations to coincide with Chinese New Year also served this purpose. An extreme measure was the lockdown of the city of Wuhan, which placed the entire population in domestic quarantine (see Measures section in the article COVID-19 Pandemic in the People's Republic of China).
Speaking on March 9, 2020, WHO Director-General Tedros Adhanom Ghebreyesus said that more than 70% of the approximately 80,000 infection cases had now recovered and left clinics. The number of new infections in China that day was 45.
The WHO mission report, for which scientists from eight countries spent nine days in the country in February, said China had launched "possibly the most ambitious, agile and aggressive disease-control effort in human history."
India
→ Main article: COVID-19 pandemic in India
On March 24, 2020, the government of India issued a 21-day curfew for the entire population because there were officially more than 500 Corona cases despite comparatively few tests. Narendra Modi, India's current prime minister, ordered particularly strict measures. Government offices, offices, shopping malls and public transport are shut down - this measure came into effect just four hours after it was announced, which meant that the population had hardly any time to prepare and food supplies were partially unavailable due to extreme hoarding. According to the International Labor Organization, 80.9 percent of the workforce in India is employed in the informal sector - without contracts, wage continuation or insurance. Every day that passes without work means a day without income for them. In addition, many have hardly any reserves.
Iran
→ Main article: COVID-19 pandemic in Iran
On February 20, 2020, Iran reported detection of the virus in two deaths. Because the numbers reported to the World Health Organization for Iran showed a higher than average number of deaths relative to the number of people infected, press reports suspect a high number of undetected or unreported infections with SARS-CoV-2. Experts expressed concern that Iran lacked the resources to contain the spread of infection should case numbers rise sharply. Travelers staying in Iran were the source of infections in several countries in the Middle East, such as Afghanistan, Bahrain, Iraq, Qatar, Kuwait, Lebanon, Oman, Pakistan, and the United Arab Emirates, until early March 2020.
On February 25, 2020, it was announced that Iranian Deputy Minister of Health Iraj Harirchi, who the day before had denied covering up the extent of the outbreak, had tested positive for the novel coronavirus. A World Health Organization team was on the ground March 2-10 to help combat the COVID-19 outbreak, warning that health care workers needed better protection. On March 4, 2020, the country's attorney general said hoarding respirators and other supplies was punishable by death.
According to the WHO report of March 23, 2020, the official number of deaths was 1,685, out of a total of 21,638 cases of infection. The highest level of new daily infections was reached on March 30, with 3,186 cases, after which the number fell steadily, so that on April 8, below 2,000 new infections per day were reported for the first time since March 24. The total death toll already surpassed that of China on April 4, and as of that date was higher in only five other countries in the world. Iran also remains among the hardest hit countries in terms of the number of people infected. As of April 10, 2020, only seven other countries reported more infections. As of May 25, 2020, WHO reported 135,701 infected and 7,417 deaths.
Turkey
→ Main article: COVID-19 pandemic in Turkey
Turkey was not affected by the COVID-19 pandemic for a comparatively long time. As a preventive measure, thermal imaging cameras were installed at international airports on January 24, 2020, and tests were conducted on travelers from China; later, all passengers were screened. On March 11, 2020, Health Minister Fahrettin Koca announced that a man who had been in Italy and Germany, among other countries, had tested positive for the virus. On March 12, a special meeting was held under the leadership of the President of the Republic. As a result, it was announced that all schools would be closed and distance learning would begin in schools on March 23. Further, flights to several EU countries were banned as a first step, followed later by Switzerland, the United Kingdom and Saudi Arabia. On March 16, 2020, all businesses that do not provide basic services were closed. By March 22, 2020, 1,236 people had been infected and 21 had died, according to the Ministry of Health. By March 31, 13,531 were infected and 214 had died, according to Health Minister Fahrettin Koca. On April 10, Turkey became the 11th country worldwide to report its 1,000th death. The number of infected people was now 47,029, eight times higher than two weeks earlier, when it was reported at 5,698. As of May 25, 2020, WHO reported 156,827 infected and 4,340 deaths.
Near East, Middle East
In the Near East and Middle East, Israel and Lebanon each reported their first case on February 22, 2020. On February 24, Kuwait (3), Bahrain (1), Afghanistan, and Iraq (1) confirmed the first cases of infection in their countries. All of these newly reported cases reportedly had links to Iran. The cases in Lebanon, Kuwait, Bahrain, Oman, Qatar, and the United Arab Emirates, as well as Iraq and Afghanistan, were subsequently found to be linked to travel to Iran. On March 22, 2020, Syria also officially announced its first coronavirus case.
Experts are particularly concerned about the possible spread of the virus in countries with inadequate healthcare systems and overcrowded refugee camps. In northwestern Syria, for example, three million refugees live in precarious living conditions, and Syria's healthcare system is largely run down after nine years of civil war.
Republic of China (Taiwan)
→ Main article: COVID-19 pandemic in Taiwan
Starting with the 2004 SARS epidemic, Taiwan established the National Health Command Center as a centralized body to manage the response to a new outbreak. On December 31, 2019, the day the PRC notified WHO of a cluster of pneumonia cases, Taiwan authorities began fever testing and surveys of all air travelers from the People's Republic. By Feb. 24, 2020, the panel had decided on 124 individual measures, ranging from quarantine regulation, proactive search for infected persons, regulations for schools and educational institutions, and sea and air border control. The production of protective masks was increased, with soldiers brought in. On January 20, 2020, the Taiwan CDC announced it had a stockpile of 44 million surgical masks and 1.9 million N95 masks (out of a population of about 23.5 million). The number of isolation rooms with negative pressure systems on standby was reported to be 1100. Taiwan summarized travel, medical, and social security data to calculate the vulnerability of individual persons. Based on this data, a real-time alert was sent to the individuals concerned via mobile phone. This only made entry possible. If the data was unremarkable, the persons were waved through. In the case of suspected cases based on the travel data, the persons concerned were immediately transferred to domestic quarantine for the duration of the incubation period. Compliance with quarantine was monitored via cell phone using the same program.
In early March 2020, it became apparent that the containment of SARS-CoV-2 in Taiwan was highly successful with these measures, although Taiwan, under pressure from China, was officially not provided with information by WHO and was almost completely excluded from cooperation.
South Korea
→ Main article: COVID-19 pandemic in South Korea
In mid-February 2020, the first cases were detected in South Korea, where it was not clear where they had contracted the disease. The number of known cases of infection hovered below 50 until February 20, 2020, when it jumped. A significant portion could be traced to a 61-year-old super-spreader who had infected at least 37 other followers within the Shincheonji Church in Daegu. She had previously refused a virus test. As of Feb. 22, 2020, more than 400 cases of infection had already been reported in the country, about half of which were linked to the church congregation in Daegu and a hospital in Cheongdo in the surrounding area, in addition to two deaths. The cities of Daegu and Cheongdo were declared "special surveillance zones" by authorities. As of February 23, 2020, there were more than 600 cases of infection, as well as five deaths. President Moon Jae-in stated that the country was at a "serious turning point." He said the next few days will be crucial in combating the spread of the viral infection. In South Korea, there are apps and websites that warn of places where infected people have been proven to have been (with their smartphones). To contain the epidemic, health authorities increased the country's testing capacity from about 200 at the end of January 2020 to about 1,000 at the end of February 2020, with about 146,000 people tested in South Korea from Jan. 20 to March 5. According to media reports, 400,000 people were tested daily in early April 2020. The goal of the mass testing program is to break the chains of infection by isolating all carriers, including symptom-free patients.
Southeast Asia
On January 27, 2020, the first case of SARS-CoV-2 was recorded in Cambodia in a Chinese man who came from Wuhan. On February 13, 2020, the cruise ship Westerdam arrived at the port of Sihanoukville. A U.S. passenger was diagnosed with the virus shortly thereafter while continuing her voyage to Malaysia. Since then, the remaining 980 passengers and crew members of the Westerdam were not allowed to leave the ship until they tested negative for the virus. However, since another 1276 passengers besides the woman had already left the ship untested and traveled on in the meantime, experts feared that the novel coronavirus epidemic would now be much harder to contain. By April 10, 2020, 120 cases had been reported, and no deaths were known at that time.
See also: COVID-19 pandemicin Cambodia
In Singapore, identification of all patients with pulmonary diseases who had previously entered from the Wuhan region and body temperature measurement of all travelers arriving from Wuhan at the airport began as early as January 2 and 3, 2020, respectively. In January, alert levels and contact tracing were gradually expanded. On January 31, 2020, entries from Hubei were banned and 700 people who had previously been in Hubei were isolated. Residents coming from China had to isolate themselves for two weeks from then on. After declaring the alert level "DORSCON orange", food and basic goods were sold out in many cases, Premier Lee Hsien Loong called on the population to be calm in a video address on social networks. There were plenty of supplies, the city would not be sealed off, and not all citizens would be ordered to stay at home, as happened in China, South Korea or Italy.
As of February 19, 2020, 84 infected persons had been treated in clinics, 4 of whom were admitted to an intensive care unit. By March 16, 2020, there were 121 confirmed COVID-19 cases; however, almost as many patients had been discharged as cured. All COVID-19 cases were isolated within a very short time, and contacts were identified and quarantined using contact tracing management developed after the SARS epidemic 17 years earlier. Premier Lee was able to announce that the situation was under control and that the city would not be shut down, as had happened in China, South Korea or Italy. Travelers from Germany were not allowed into the country, the country was considered a risk case - as one of those countries that had not taken COVID-19 seriously enough for too long, as Premier Lee criticized: "An alarming level of inactivity is what the World Health Organization has called it. We here in Singapore have taken COVID-19 absolutely seriously from the beginning." As of April 15, 2020, there were 3699 infected people, including 10 deaths.
See also: COVID-19 pandemic in Singapore
Thailand reported the first SARS-CoV-2 case outside of China on January 13, 2020. By April 15, 2020, the number of infected persons had increased to 2672, including 46 deaths.
See also: COVID-19 pandemic in Thailand
Japan
→ Main article: COVID-19 pandemic in Japan
The number of infected persons on or off board the Diamond Princess in Yokohama Port rose to 691 on February 24, 2020. These cases of infection are not attributed to Japan in WHO reports but are listed as international carriage (see the Charts and Tables section). On February 26, the education bureau in Hokkaidō Prefecture ordered elementary and middle schools to close for several days. On the same day, the number of infections in Japan rose to 164. The following day, Prime Minister Shinzō Abe announced the closure of all schools in Japan by April 2020; exceptions were made for children whose working parents had no childcare options. By mid-March, there were about 800 infected and a dozen deaths; by mid-April, more than 10,000 infected and more than 100 deaths; and by mid-May, more than 15,000 infected and more than 700 deaths.
Australia and Oceania
→ Main article: COVID-19 pandemic in Australia
→ Main article: COVID-19 pandemic in New Zealand
Europe
→ Main article: COVID-19 pandemic in Europe
There have been confirmed corona infections in Europe since January 16, 2020. A week later, on January 24, 2020, the first case on the European continent was reported to WHO in France, and on January 25, the first death outside Asia was reported, also in France. Due to the high numbers, which exceeded those in China, WHO classified Europe as the epicenter of the pandemic in early March 2020.
By April 2021, the continent had experienced three waves of the pandemic. The first lasted from March to May 2020; it led to an overload of health infrastructure in many countries, resulting in high mortality. The second wave occurred from September 2020 to early February 2021, and the third followed shortly thereafter, beginning in March 2021.
Africa
→ Main article: COVID-19 pandemic in Africa
On February 14, 2020, the first case of infection on the African continent - in Egypt - was reported. It involved a 33-year-old patient originating from abroad; according to the Egyptian Ministry of Health, all his contacts tested negative for the pathogen. As of March 16, 2020, cases had been reported by 26 African countries. Angola reported its first Corona case on March 21, 2020. As of March 25, 2020, 2412 cases have been reported in 43 African countries, including 709 in South Africa.
North America
Canada
→ Main article: COVID-19 pandemic in Canada
On March 13, it was announced that the wife of Canadian Prime Minister Justin Trudeau had tested positive. As a precaution, both went into domestic quarantine for 14 days. Trudeau was the first head of government to go into domestic quarantine.
Numerous measures against the virus have been announced. Parliament is to close for five weeks, international flights are to be diverted to a small number of airports with special controls, and cruise ships with more than 500 passengers are to be banned from docking. An entry ban was initially refrained from in order not to give rise to illegal border crossings. The government called on citizens to refrain from expendable foreign travel and to stay away from crowds in the spirit of spatial distancing. On March 16 and 18, respectively, entry bans were imposed after all.
United States
→ Main article: COVID-19 pandemicin the United States
The first confirmed case in the U.S. was reported from Washington State on January 21, 2020. As of March 6, 2020, 245 confirmed cases and 14 deaths were known. Domestic quarantine has been imposed on numerous people in several states, notably more than 2,500 people in New York alone and more than 9,700 in California (as of March 6, 2020). These are contacts of the first confirmed infected persons as well as returned travelers.
In late January, CDC assessed the risk from COVID-19 to the U.S. population as low.
The Federal Reserve placed dollar bills returning from Asia under a seven-day quarantine in March 2020.
Initially, U.S. President Donald Trump downplayed the dangers of the novel coronavirus. Numerous statements made by Trump in the first two weeks of March on the pandemic turned out to be incorrect in retrospect and are therefore denounced by CNN as "false statements". In a televised address on March 11, 2020, he announced - without consultation with the EU - a one-month ban on the entry of non-U.S. citizens who had been in any of the 26 European countries in the Schengen Area during the previous two weeks. A few days later, Trump extended the entry ban to the UK and Ireland.
In light of the spread of novel coronavirus in the U.S., a national emergency was declared on March 13, 2020. By then, fewer than a total of 15,000 people had been tested - with around 2300 testing positive for COVID-19. This comparatively low number of people testing positive for COVID-19 was due to a lack of testing. Many people with symptoms of the disease failed to get tested. President Trump stated that production of five million coronavirus tests was targeted and would be available "very soon."
California became the first U.S. state to impose a curfew on March 19, 2020. Governor Gavin Newsom assumed that almost 60 percent of the 40 million inhabitants could become infected in the next eight weeks. In some parts of California, Newsom said case rates had previously doubled every four days. Up to the imposition of the curfew 958 cases of infection had become known in California as well as 19 deaths. On the same day, Mayor Eric Garcetti had called on Los Angeles residents to stay home if possible. Earlier, in the San Francisco area, many counties had already faced a week-long curfew.
On March 27, 2020, over 100,000 infected persons were reported in the USA for the first time. This made the USA the new center of the pandemic, alongside Europe and after China. On April 4, the U.S. health authority CDC called on the American public to wear protective masks in everyday life to slow the spread of the infectious disease.
Latin America
The COVID-19 pandemic reached Latin America later than Asia and Europe. Since then, however, the virus has spread across all countries in the region, albeit at different rates and with different numbers of infections and deaths. In many countries, health systems are overwhelmed. The response of Latin American governments has also varied. While states such as Argentina, Bolivia, Colombia, and Uruguay ordered early spatial distancing as part of a mass quarantine, the presidents of Mexico and Brazil (see Misinformation on COVID-19 Pandemic #Brazil) initially downplayed the threat posed by the virus. Rapid social relief measures were adopted in many states. In many cases, governments were given special powers. Even in cases where this seems justified to contain the pandemic, critics fear a loss of democratic quality and the legitimization of authoritarian practices beyond the acute crisis.
Brazil
→ Main article: COVID-19 pandemicin Brazil
After the first confirmed infection with the novel coronavirus was reported from South America on February 26, 2020, in Brazil, and two positive cases were reported from Mexico on February 28, there were 10 additional confirmed SARS-CoV-2 infections in Latin America as of March 1, 2020: a second case in Brazil, four cases in Mexico, six in Ecuador, and one case in the Dominican Republic. By March 8, five confirmed cases of infection had been added in Costa Rica. On the South American continent, infections also occurred in Peru, Colombia, and French Guiana.
The two Brazilian first-time patients, a 61-year-old and a 32-year-old, were from São Paulo and had recently returned from trips to Italy. On April 4, 2020, the country officially reported 10,278 infections; a week later, the number doubled. In addition, the thousandth death was reported on April 11, 2020.
Ecuador
→ Main article: COVID-19 pandemic in Ecuador
The country most affected initially in Latin America was Ecuador. By March 4, the number of people confirmed infected there had risen to ten. All cases are contacts of a 71-year-old woman living in Spain who traveled to Ecuador from Madrid and became ill a few days after arriving. By March 8, the number of confirmed cases of infection in the country had increased to 14, and by April 7, Ecuador had 3747 infections. Of these, 1600 infected people were in hospitals alone due to a lack of protective materials.
Ecuador has significantly more infected and dead relative to the total population than the other Latin American countries. As of March 15, there were already 10,000 more deaths in the hardest-hit province of Guayas than had been counted in normal years up to that point, so it can be assumed that the virus appeared much earlier than previously known. In the Ecuadorian metropolis of Guayaquil (Guayas Prov.), the burial system collapsed at the end of March. Special forces had to begin a three-week recovery mission and by April 12 had retrieved 1402 bodies from private homes and hospitals in the city, as the morgues were full and some of the dead were dumped in the streets; in addition, other bodies had been privately cremated earlier without being examined. The official death toll of just over 300 at that time must therefore be considered unrealistic and a high number of unreported cases must be assumed. However, the cause of the respective deaths of the recovered corpses was not disclosed, so that no reliable figure can be determined any longer.
Cuba
→ Main article: COVID-19 pandemic in Cuba
On March 11, Cuba reported its first cases; three tourists from Italy tested positive for COVID-19. The spread of the SARS-CoV-2 virus in Cuba is testing the socialist Caribbean island's health care system. Originally brought to the island by tourists and Cubans traveling back from abroad, the virus has spread rapidly throughout the island, with about 1,000 cases of infection counted as of mid-April. The country has a broad health care system with a very high density of doctors (see COVID-19 pandemic in Cuba). At the same time, medical care suffers from a lack of equipment and medicines as well as low wages for staff. In addition, there are sometimes dramatic supply bottlenecks, including for sanitary products and the water supply. Due to the high age structure, about a quarter of the population is considered a risk group. Despite the critical situation on the island itself, Cuba sent medical brigades to fight the COVID-19 epidemic in other countries, including northern Italy and numerous Caribbean states.
Cuba's difficult economic situation is exacerbated by the pandemic, which has led to the collapse of the country's main economic sector, tourism. The government has taken lock-down measures. To provide emergency supplies to the population, it has increasingly withdrawn food and sanitary products from free sale and transferred them to the distribution economy of the rationing system.
Antarctica
In December 2020, 36 SARS-CoV-2-infected personnel were recorded at Chile's Bernardo O'Higgins Station on the Antarctic Peninsula, including 26 members of the military and 10 civilian personnel. These were the first known cases of the COVID-19 pandemic on the Antarctic continent.
Refugee camps and marginalized Roma settlements
→ Main article: Impact of the COVID-19 pandemic #Refugee camps and marginalized Roma settlements.
The experts are particularly concerned about the possible spread in countries with inadequate health care systems, overcrowded refugee camps and marginalized slum settlements, in which members of the Roma national minority in particular have to live in many countries. When dealing with the at-risk group of Roma cumulating in slum settlements, ethnic discrimination and consequent unequal treatment add to the difficulty. In some countries, Roma settlements are sealed off by the police and, when individual Roma are quarantined, strict measures are imposed on the entire Roma collective, while measures are taken against members of the majority population only on an individual basis. The health protection of the Roma is neglected in the process.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in Cuba according to WHO data; top cumulative, bottom daily values.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in Brazil according to WHO data; top cumulative, bottom daily values.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in the United States according to WHO data; top cumulative, bottom daily values.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in Japan according to WHO data; top cumulative, bottom daily values.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in Egypt according to WHO data; top cumulative, bottom daily values.

People check at the city border of Xi'an in central China's Shaanxi province, late January 2020.

Doctor in protective suit interviewing patients at Wuhan hospital in January 2020
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in India according to WHO data; top cumulative, bottom daily values.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in Israel according to WHO data. Top cumulative, bottom daily values
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in South Korea according to WHO data; top cumulative, bottom daily values.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons in the People's Republic of China according to WHO data; top cumulative, bottom daily values.
Global trends in SARS-CoV-2 infections by country from January 12, 2020, to February 29, 2020.
_-_Infizierte_(800px).svg.png)
Confirmed infected persons worldwide according to WHO data; top cumulative, bottom daily values.
_-_Tote_(800px).svg.png)
Confirmed deaths worldwide according to WHO data; cumulative above, daily values below.
National measures
Numerous countries adopted more or less drastic quarantine measures such as contact restrictions, curfews, school closures, and travel and accommodation restrictions. A large wave of such measures was adopted worldwide in March 2020. Many states then relaxed quarantine measures again in May and June 2020. In addition, states are working to strengthen their health systems, procure protective equipment, fund research on COVID-19 treatment and vaccine development, and take other pandemic prevention measures. Finally, following the quarantines, governments took action to overcome the 2020 economic crisis. National actions vary widely, depending on governments' policy priorities and available resources. For more detailed information, see the articles on the COVID 19 pandemic in individual countries.
Countries with successful pandemic protection measures in 2020
- Australia
- New Zealand
- Taiwan
- China
- American Samoa
- Tonga
- Tuvalu
World map on curfews and school closures
Measures for collecting contact and transaction data
COVID-19 apps
→ Main article: COVID-19 app
COVID-19 apps are mobile apps designed to help contain the COVID-19 pandemic through contact tracking. Many countries are developing their own apps, some on the same standards, to achieve compatibility.
Other evaluation of location data
Even without tracking apps, the tracking capabilities of cell phones and the movement profiles derived from them can be used to check whether citizens are complying with the legal norms issued in the context of the coronavirus pandemic, "whether the population is adhering" to the recommendations to "stay at home," for example. Lothar Wieler, the president of Germany's Robert Koch Institute, explained that the information needed for this, tracking and movement data, is provided by Deutsche Telekom: It is possible, he said, "to track on a small scale and fairly up-to-date how certain measures that have been introduced to combat epidemics are also having an effect." With mobility data, for example, it is possible to observe on a daily basis "how people move and whether they have changed their behavior in recent weeks.
Overview of various national measures
Overview of exit restrictions (as of June 7, 2020)
Countrywide adopted exit restrictions (active).
Decentrally or regionally decided output restrictions (active)
Countrywide exit restrictions that no longer exist
Regional output restrictions that no longer exist
No output restrictions
School closures of the respective countries decided due to COVID-19 (as of June 7, 2020).
Regional school closures
Statewide school closures
No school closures
No data
International measures
International health emergency, WHO action
On January 30, 2020, WHO Director-General Tedros Adhanom Ghebreyesus declared the existence of a public health emergency of international concern (also known simply as an "international health emergency"). This was prompted by concerns about the possible spread of the viral epidemic to countries with poorly developed health systems, particularly in sub-Saharan Africa. The director-general of the World Health Organization explicitly emphasized that the health emergency had not been declared because of the situation in China. He said that WHO continues to have full confidence in China's ability to control the epidemic in the country.
On February 11 and 12, 2020, a conference was held in Geneva at the invitation of the World Health Organization, where more than 400 experts from various disciplines deliberated on the epidemic. The aim was to share knowledge about the COVID-19 disease and the SARS-CoV-2 virus that causes it, and to define timely strategies for developing vaccines and treatments. Speaking at the Munich Security Conference on Feb. 15, 2020, Ghebreyesus said Chinese measures helped slow the spread of the epidemic to other countries. He praised the good cooperation of international research groups and said that tests to diagnose the virus and personal protective equipment for medical personnel have been sent to states with great need. WHO's Situation Report-29 of February 18, 2020, reported that test kits for laboratory diagnosis of COVID-19 had been shipped to 56 states, as well as more than 12 tons of personal protective equipment to states with special needs in the Western Pacific, Southeast Asia, and Africa regions. On March 13, 2020, the WHO Director-General reported that 1.5 million test kits had been shipped to 120 states, with 28 more to follow, and supplies of personal protective equipment had also been provided to 56 states. The April 7, 2020, WHO Situation Report - 78 update listed more than 900,000 mouth-nose protective masks, 62,000 N95 masks, 1,000,000 protective gloves, 115,000 gowns, 17,000 goggles, and 34,000 face masks shipped to 133 states.
According to media reports, the WHO Director-General said on February 24, 2020, that so far it is not a pandemic, but epidemics in individual countries, because so far there is no uncontrolled global spread of the virus. To speak of a pandemic would stir up fear, was in principle irrelevant and would not save lives.
On March 1, 2020, WHO issued a recommendation for the use of personal protective equipment. This was motivated by the global shortage of protective clothing, which already exists for respirators and is foreseeable for gowns and eye protection. It recommends the use of mouth-to-nose protection when providing direct patient care, including. FFP2 or N95 masks should be worn longer and on multiple patients to save material. These higher-quality masks should be used only for aerosol-forming procedures on patients. General population use of masks was recommended only for family caregivers and individuals with respiratory symptoms. In several states at the same time, shortages occurred that could not be compensated for in the short term by production increases and conversions. Shortages of protective medical clothing, including respirators in particular, as well as oral and nasal protection for healthcare professionals and the general public, and disinfectants, became factors that governments had to factor in when weighing options. In some cases, governments intervened directly in production decisions and supply chains.
On March 11, 2020, WHO officially classified the global spread of the coronavirus as a pandemic. WHO Report 53, issued on March 13, 2020, announced that the COVID-19 Solidarity Response Fund has been established in collaboration with the UN Foundation and other partners to address the pandemic. The goal is to raise $675 million by the end of April to support states with special needs in their efforts to combat the spread of COVID-19. To raise funds for the Solidarity Fund and recognize healthcare workers in the global effort against the novel coronavirus, a live global streaming and TV event, "One World: Together At Home," has been planned for April 18 in conjunction with the NGO Global Citizen. The event is curated by Lady Gaga and will feature contributions from international artists and leading health experts.
In early April 2020, WHO supported six eastern members of the WHO Europe Group with funding of 140 million euros, of which 30 million euros came from the EU Commission. The funds were used for medical equipment, personal protective equipment and diagnostic tests, as well as training for medical and laboratory staff and information campaigns in Armenia, Azerbaijan, Georgia, Republic of Moldova, Ukraine and Belarus.
WHO also published information on individual prevention, based on the latest scientific evidence. On April 29, the recommendations were:
- regularly and thoroughly wash hands with soap and water or with a hand washing lotion suitable for hand disinfection, or wet hands with an alcohol-based hand disinfectant;
- keep at least 1 m distance to other persons;
- Avoid crowded public places;
- if possible, do not touch the eyes, nose or mouth;
- sneeze or cough into the crook of your arm or into a handkerchief;
- stay at home when you feel sick;
- consult a doctor in case of fever, cough and shortness of breath (call first before visiting);
- stay at home even if symptoms are mild (such as a slightly runny nose or headache)
COVAX is one of three pillars of the Access to COVID-19 Tools (ACT) to accelerate "access to COVID-19 tools" established in April 2020 by the World Health Organization (WHO), the European Commission, and France in response to the COVID-19 pandemic. WHO, in collaboration with the Global Alliance for Vaccines and Immunization (GAVI) and the Coalition for Epidemic Preparedness Innovations (CEPI), has also implemented COVAX to coordinate global vaccine development. 184 countries have joined COVAX to date, of which 92 economies that cannot afford the vaccine due to low and middle incomes are eligible to access COVID-19 vaccines through Gavi COVAX Advance Market Commitment (AMC) (as of November 12, 2020). Ensure that each participating country receives a guaranteed share of doses to vaccinate the most vulnerable 20 percent of its population by the end of 2021.
On June 1, 2021, the IMF, WHO, World Bank, and WTO presented a joint plan for more equitable access to immunization and called on the international community to support, implement, and promote with new financial resources a strengthened and coordinated global immunization strategy.
Measures in the EU
In a survey of 47 laboratories completed on January 29, 2020, the European Centre for Disease Prevention and Control (ECDC) identified testing capacity within the European Union (EU) at 8275 per week at 37 laboratories in 24 states. This capacity should be increased to 9150 tests per week at 46 laboratories by February 17, 2020.
At a meeting of EU health ministers in Brussels on February 13, 2020, it was decided to work closely together to ensure information exchange, procurement of personal protective equipment, and necessary capacity in treatment and diagnosis of COVID-19. Funding was allocated for research and development of a vaccine. EU-wide entry requirements were not agreed upon, but plans were made for travelers from certain regions to be questioned about their contacts with people from areas affected by the epidemic. At the meeting, German Health Minister Jens Spahn rejected national go-it-alone measures, as well as the taking of fevers from people entering the country.
On February 24, 2020, the European Commission announced aid investments of 232 million euros. The money is earmarked for the WHO, for research, for Africa and for flights for the repatriation of EU citizens.
On March 12, 2020, the European Central Bank (ECB) decided to make 120 billion euros available by the end of the year for long-term loans for banks and the purchase of securities. A week later, the ECB announced further bond purchases of 750 billion euros until the end of the year, with which it intends to stabilize the economy.
The EU Commission adopted guidelines on March 16, 2020, in which it called on member states to ensure the unimpeded movement of goods in the European single market as far as possible during border controls, as well as free border crossing for commuters working in the health and food sectors. EU citizens who want to go home through another country should be facilitated in their transit, it said.
On March 17, 2020, the heads of state and government of the European Union decided on a 30-day entry ban for non-EU citizens that will take effect immediately. There are exceptions for people with a longer-term right of residence in an EU state and special arrangements for citizens of EFTA states and the United Kingdom. Those who have an urgent reason for entering the country (for example, a funeral or a court appointment) would have to carry the relevant proof.
The EU Commission announced on March 20, 2020 that it would relax budget rules because of the Corona crisis. For the first time, the general escape clause of the EU Stability Pact will be activated. This means that "national governments can pump as much liquidity as necessary into the economy".
At the beginning of March, export embargoes for protective equipment, especially respiratory masks and protective clothing, were imposed in some countries, such as Germany and France. As a result, deliveries were held back for countries that were already severely affected, such as Italy, Switzerland and Austria. The EU Commission had to issue a reprimand for lack of solidarity. It was not until mid-March 2020 that an agreement was reached, which amounts to joint procurement by the Commission and export restrictions only for EU third countries. China announced that it would supply Europe with material now no longer needed there. However, many of these Chinese supplies later turned out to be in short supply.
German Chancellor Angela Merkel praised the initiatives of the EU Commission, for example on the joint procurement of protective clothing.
In a survey by the market research service Aposcope, 32.1% of 56 pharmacies surveyed said they charged a markup of 40% to less than 50% when selling the masks; 16.1% charged a markup of 50% or more. According to the Bavarian Pharmacists Association, the purchase price for surgical masks was previously a few cents and has risen to between one and two euros since the transition to mandatory masks. The Federal Association of German Pharmacists pointed out that the professional code of conduct for pharmacists forbids "overly offensive pricing, vulgo 'usury'".
In a video summit meeting of member states' leaders on March 26, 2020, some participants, as well as many economists before them, took the position that states should issue common bonds to fight the crisis (also known as "corona bonds"). However, no agreement was initially reached on a common position on financing crisis response measures. The president of the European Research Council, Mauro Ferrari, submitted his resignation on April 7, 2020, out of disappointment with the EU's response to the crisis.
On April 9, 2020, the EU decided as a first aid measure to grant loans from the euro rescue fund ESM up to an amount of 240 billion euros to member states particularly affected by the pandemic, to provide loans from the European Investment Bank (EIB) in the amount of 200 billion euros for companies and to set up a short-time working program called "SURE" (Support Mitigating Unemployment Risks In Emergency) with a volume of 100 billion euros. A longer-term, second aid package of the same amount (a so-called Recovery Fund) was agreed, but for the time being no agreement was reached on concrete financing.
The European Group on Ethics in Science and New Technologies (EGE), which has an advisory role to the European Commission, issued a statement in April 2020 on European solidarity and the protection of fundamental rights during the COVID-19 pandemic. It called for solidarity not to be limited to one's own region or country, pointing out that socioeconomically worse off people are more affected by the pandemic. The effects - the economic downturn as well as an increase in domestic violence, child abuse and suicides - should be addressed through immediate support measures of a financial and psychosocial nature, starting from the equal value of all people based on human dignity. Specifically, build on the financial assistance tools used to address the 2008 financial crisis; EU member states that have greater medical resources should share them. Saving human lives was the first goal, while at the same time ensuring that the crisis was not used to abuse power. Surveillance data should be deleted at an early stage after proportionality has been weighed. After the crisis, the experience gained should be used to develop a joint strategy for dealing with future threat situations.
On May 18, 2020, Angela Merkel and Emmanuel Macron surprisingly presented a joint proposal for a reconstruction fund. Instead of joint and several liability as with "corona bonds," the aid of 500 billion euros is to be financed via the EU budget. This would also allow direct democratic control of the use of funds.
The future European Health Emergency Response Authority (HERA) is to be created within the framework of a European Health Union as a European authority for emergency measures in the health sector. Triggered by the problems encountered in combating the COVID 19 pandemic, the European Commission on November 11, 2020, defined the main elements of the future authority, which is to be operational from the end of 2021.
Foreign policy and foreign policy international cooperation
Air travel and tourism
→ Main article: International traffic in the COVID-19 pandemic #Air and travel traffic.
Between 12,000 and 15,000 commercial aircraft remained grounded worldwide in April 2020. A Credit Suisse analyst expected civil aviation revenue to decline by 90 percent year-on-year in July 2020.
Individual cruise ships affected
→ Main article: Ships under quarantine in the COVID-19 pandemic.
Several cruise ships were quarantined as part of the COVID-19 pandemic, and others had to change their routes to dock at another port due to fears that the virus would spread further on land. Several states brought their citizens who were stuck on quarantined cruise ships back home. In part, the handling of quarantine measures on board and around disembarkation was assessed as a risk for increased spread of the virus.
Evacuations
→ Main article: International transport in the COVID-19 pandemic #Evacuations.
World Bank
Having already launched a $12 billion aid package in March 2020 to help developing countries fight the coronavirus, the World Bank announced in April 2020 that it would provide $160 billion.
The World Bank had launched the Pandemic Emergency Financing Facility (PEF) in 2017 as an insurance market for global pandemic emergencies, in collaboration with reinsurers Swiss Re, Munich Re and GC Securities. Bonds totaling $320 million were issued. These yield high interest annually, in return for which investors lose part or all of their deposit if the conditions for a pandemic are met. The money is then used to fund the crisis response. According to media reports, this happens 84 days after a corresponding situation report by the WHO. In part, it is difficult even for well-informed investors to estimate when the pandemic emergency will occur. The bond, which is not traded on public exchanges, lost much of its value in the wake of the coronavirus epidemic crisis. Experts emphasize that the amount is small compared to the World Bank's total liquid assets of ten billion dollars.
United Nations
United Nations Secretary-General António Guterres on March 23 called for an immediate global ceasefire to protect civilians in conflict regions from the pandemic. Guterres later said his call has since been endorsed by 70 states as well as regional partners, non-state actors, civil society networks and organizations. Among them, he said, are 11 states embroiled in long-standing conflicts. An online petition referring to this UN call was supported by more than one million people.
The United Nations issued its first joint resolution on the COVID-19 pandemic on April 2, 2020. In it, they called for greater international cooperation and multilateralism, urged the protection of human rights, and spoke out against discrimination, racism, and xenophobia. Some states, including Russia, had called in advance for the suspension of international sanctions as well. The media criticized the United Nations' late response to threats to international peace and security as a "gap between standardized aspirations and reality."
On April 15, 2020, the UN agencies IOM, UNHCR, and UNICEF welcomed Luxembourg's acceptance of unaccompanied refugee minors from Greece.
The Alliance for Multilateralism pledged its support to the United Nations, WHO, and other international organizations for their efforts to contain, combat, and prevent the spread of the pandemic in an April 16, 2020 joint statement signed by the foreign ministers of numerous countries.
Media reported a May 8, 2020, U.S. veto of a previously negotiated compromise proposal for a COVID-19 resolution. This was intended to support a global ceasefire in the pandemic. The United States objected to the naming of WHO in the draft, which had been prepared by France and Tunisia. Nor did they agree to a draft that had been modified in its wording.
International non-governmental organizations
A number of international nongovernmental organizations (NGOs) were working to combat the virus in Wuhan, including Project HOPE, Direct Relief, and Save the Children China.
The National Red Cross Societies work as national relief societies in close cooperation with authorities to combat the virus.
Médecins Sans Frontières (MSF) works to help vulnerable populations in countries including Italy, Spain, Belgium, France, Switzerland, Norway and Greece. In Italy, about 30 MSF staff provide support to hospitals, nursing homes, and patients, and help primary care physicians and health professionals implement home-based isolation (as of March 27, 2020). In Spain, MSF set up temporary hospitals where patients with moderate symptoms can be treated to relieve pressure on emergency rooms and intensive care units, and provides advice on protecting health workers and the elderly. In France, MSF supports local health authorities in diagnosing and treating infections in vulnerable populations, particularly among migrants and the homeless.
Research institutions and universities
- The publishers of several major medical and scientific journals have published scientific papers on COVID-19 in a timely and fully open-access manner to facilitate direct access to the current state of the science for medical professionals and researchers: for example, The Lancet journals published by Elsevier, the Journal of the American Medical Association (JAMA) published by the American Medical Association (AMA), The New England Journal of Medicine (NEJM) published by the Massachusetts Medical Society, or Nature published by the Springer Nature publishing group. WHO established a bibliographic database.
- Research is taking place on the one hand in the areas of vaccine development and for the treatment of sick people, and on the other hand in diagnostics to detect active disease and antibody tests to detect infection that has already occurred. Important preliminary work for vaccine development was the decoding of the genome of the virus isolated in Wuhan in January 2020, published in the open-access GenBank of the National Center for Biotechnology Information, followed by the decoding of other genome sequences. Advances in diagnostics and antibody testing are improving the traceability of the disease and thus can help flatten the progression curve through adapted infection control measures, which is important to keep the number of ICU patients below the capacity limit of ICU beds. As recently as January 2020, initial detection methods for SARS-CoV-2 (then referred to as 2019-nCoV) using reverse transcriptase-polymerase chain reaction (RT-PCR) were published, and additional groups of scientists published their developed methods; they are available on the WHO website.
- Researchers developed, enhanced, and supplemented various software to mitigate the pandemic, better understand the SARS-CoV-2 viruses, contain the spread of COVID-19, and evaluate or better implement possible countermeasures - such as potentially repurposed medical countermeasures.
- As part of research collaborations, to accelerate decoding of the SARS-CoV-2 virus and research into treatments, the computing power of the following supercomputers, Oka Ridge Summit, Sierra and others, is being pooled in the COVID-19 High Performance Computing Consortium. The total computing power is 600 petaflops, supported by 6.8 mill CPU cores, 50,000 graphics processors and 165,000 network nodes. The Folding@home project serves the same purpose.
- Researchers at Switzerland's Eawag and EPF Lausanne succeeded in detecting traces of the SARS-CoV-2 virus in wastewater at the end of April 2020. In samples taken daily from the Lausanne wastewater treatment plant, they were able to roughly trace the increase in SARS-CoV-2 viruses in wastewater in March and April. The research success makes it possible to detect any resurgence of infections about a week sooner than on the basis of the tests. The goal is to monitor the wastewater of about 2.5 million people from about twenty large wastewater treatment plants geographically well distributed across Switzerland as part of an early warning system.
- In Germany, there has been less investment in the development of drugs against the virus, especially compared with the United States. Investments have been directed primarily toward the development of vaccines.

COVID 19 test kit
Impact
In turn, the measures adopted nationally as well as internationally had drastic effects on a large number of areas of life, which are briefly listed below and described in more detail in the respective main articles.
Socio-economic impact
→ Main article: Socioeconomic impact of the COVID-19 pandemic.
The pandemic had a far-reaching economic impact, first in China and Asia and later worldwide.
The quarantine of entire regions and exit restrictions for the population affected the supply situation and sometimes led to hoarding purchases of non-perishable foodstuffs and toilet paper in the retail sector. Service industries such as tourism, gastronomy and entertainment were also affected, suffering severe losses in sales. The disruption of cross-border supply chains led to at least temporary production stoppages. In March 2020, the stock markets of many countries crashed. The economic crisis in 2020 was also referred to in the media as the corona recession. The International Monetary Fund noted in October that this impact was not only caused by lockdowns, but also by the voluntary behavior of the population in the event of persistently high infection rates without a lockdown. According to the report, early lockdowns were shown to be more economically effective than long-term mild measures. The short-term costs of the lockdown were lower than the long-term costs. At the same time, the measures were shown to have a greater impact on women and younger people.
The pandemic has far-reaching sociocultural effects, such as on the world of work and school. As people are encouraged to carry out their work from home wherever possible (home office), negative health side effects may occur (see mass quarantine #evaluation of the measure). In connection with home office, it has been decided in Germany that employers are obliged to offer home office, unless there are operational reasons to the contrary. As a result of the pandemic, however, there was also short-time work and layoffs. In addition, there were regional or nationwide school closures. The COVID-19 pandemic also had an impact on social interaction; for example, after the call for a standoff, there were ovations at windows and balconies to thank medical personnel for their work during the crisis. In some cases, however, there was also discrimination, racism, and exclusion of people who were merely suspected of being able to transmit the novel coronavirus. In part, the pandemic has also had psychological consequences, such as fears and interpersonal problems. A lot of misinformation about the COVID-19 pandemic is circulating, especially on the Internet.
In almost all affected countries, but especially in those with mass quarantine measures or other exit restrictions or contact bans, cultural events such as theater, concerts, cinema, museum visits and sightseeing have come to a virtual standstill. This also includes church fairs, fairs, town and village festivals. Numerous movie releases were postponed, award ceremonies and festivals were canceled. Numerous sporting events were canceled or postponed because of the pandemic; initially, events in China were affected, later in Asia and, as the pandemic progressed, worldwide.
Among the victims of the pandemic are also numerous celebrities (see here: List of fatalities of the COVID-19 pandemic).
Impact on public transport
During the pandemic, a minimum public transport service was maintained in many countries. Disinfection and cleaning measures were stepped up, and cashless payment and e-ticketing were extended in many cities.
Worldwide, public transport ridership declined. The World Resources Institute, for example, referred to a report indicating a decline of 50 to 90 percent. This resulted in a loss of revenue. In Europe, the sector expects to lose 40 billion euros in 2020 due to declining ticket sales. Associations such as the International Association of Public Transport argued for government support, as public transport is seen as a key factor for the economy and social development. The World Economic Forum also advocated a modernization and digitization offensive to better cope with changing passenger behavior.
Effects on the political establishment
The illness of high-ranking politicians and preventive and quarantine measures changed the governance of some countries; in particular, the exercise of parliamentary democracy posed challenges to the states.
According to the International IDEA, as of May 2020, 50 national and regional elections and referenda have been postponed worldwide. The question of how to exercise the right to vote during the pandemic led to numerous discussions and disputes. "The elections themselves thus become a political issue," judged Der Standard from Vienna.
The UN Climate Change Conference 2020 has been postponed by one year to November 2021.
Impact on the environment and resource consumption
→ Main article: Environmental impact of the COVID-19 pandemic.
Extensive restrictions on economic activities worldwide and on individual mobility such as global tourism led to a decline in pollution and carbon dioxide emissions in many regions of the world: Earth Overshoot Day ("Earth Overshoot" or "World Overshoot Day") moved back nearly a month from July 29 of the previous year to August 22, 2020.
Other health care implications.
→ Main article: Impact of the COVID-19 pandemic on health care.
Beyond the direct consequences of the disease, the pandemic had numerous medical impacts, such as postponing planned surgeries that were not deemed necessary to free up hospital capacity.
The WHO warned against neglecting the fight against other diseases during the pandemic, such as the fight against malaria in sub-Saharan Africa. Since COVID-19 patients are often given antibiotics to treat secondary infections, this could accelerate the spread of antibiotic resistance, which has already been increasing for years.
Impact on research and teaching
The pandemic led to drastic restrictions on academic exchange. In order to maintain social distancing, numerous academic research projects were shut down. For example, an article in the Radiological Society of North America reported on possible consequences measures for radiology. Difficulties are seen in resuming interrupted clinical trials.
On the other hand, there was an intensified international exchange of information and research results on the SARS-CoV-2 virus, the course of the COVID-19 disease, and epidemiological issues.
The pandemic led to restrictions in academic teaching. For example, semesters abroad were suspended and teaching was switched to online communication.
Impact on art and culture
The pandemic has had a massive impact on almost all areas of culture and art through
- the cancellation of all presence events necessary in case of lockdowns
- the lower visits to museums, exhibitions and the like,
- Loss of income for employees in the cultural sector and freelance artists.
The lack of recreational opportunities also has repercussions in other sociocultural areas, such as demotivation in education and work, as well as other psychological consequences. Furthermore, the absence of cultural events increases the tendency toward physical inactivity, which can cause long-term damage to health.
The effects of the loss of income are countered in many states by financial subsidies or tax relief, while the other damage is more difficult to mitigate. One example of this is Aktion Neustart Kultur - a program launched by the German government in the summer of 2020, with a budget of two billion euros to preserve the cultural sector and its endangered infrastructure. Many artists offered live streams from empty venues due to large-scale event cancellations. This led to a large supply of digital artworks such as the concert film series WeLive - Das Musikfestival or the Klangspektrum BW. New compositions created as a result of the pandemic include, for example, the Missa brevis in tempore coronae for soprano solo and organ by Robert Mehlhart.
Protests
Since 2020, there have been demonstrations in some European cities because of the restrictions on everyday life (mandatory masks, lockdown, etc.) imposed by legal norms. On January 25, 2021, there were violent demonstrations in Dutch cities because of the corona-related early closing time in the catering industry; in some cases, military police were deployed. In Amsterdam, numerous stores were looted. There were many injuries and arrests. The Dutch police spoke of "the worst riots in 40 years." Riots also occurred in Tilburg, Enschede, Venlo, Roermond, Breda, Arnhem and Apeldoorn. On the evening of the following day, riots broke out again in several cities in the Netherlands because of the curfew.

Due to hoarding purchases, various products such as rice, pasta, canned goods and toilet paper were temporarily sold out
Controversies
Since the pandemic touches almost all areas of life worldwide, many social and political debates took place gradually. These are presented in the respective country articles, in the article Impact of the COVID-19 pandemic, or in the main articles of the individual topics, such as the state of the science in the article on the SARS-CoV-2 virus and in the article on the COVID-19 disease, the debate on the recommendation to wear protective masks is discussed in the article Mouth-nose protection, the debate on the collection of contact or movement data for epidemiological tracing of infection chains and the development of corresponding programs in Contact Tracing and Contact Tracing App. Fringe opinions, science denial, and problematic debate contributions are addressed, as are false claims, fake news, pseudoscientific health recommendations, and conspiracy theories, in the article Misinformation on the COVID-19 Pandemic. In the following, only the international debates and controversies that relate directly to the pandemic as a dangerous disease are presented here.
Timing of the WHO pandemic declaration
As early as February 2020, voices were raised that spoke of an emerging pandemic. At a joint lecture by the Charité and the London School of Hygiene and Tropical Medicine at the Berlin Museum of Natural History on February 26, 2020, virologist Christian Drosten said he believed it was possible that the outbreak of the new coronavirus could not be contained and would become a pandemic. Microbiologist Alexander S. Kekulé of the University Hospital Halle (Saale) expressed the opinion in Time on February 25, 2020: "At the latest with the current transmission chains in Italy, which went through several stages and cannot be traced back to an import, all criteria of a pandemic are fulfilled." Marlen Suckau-Hagel, head of the health department at the Senate Department of Health in Berlin, said in mid-February 2020: "The WHO is avoiding declaring a pandemic, but that's more of a political statement; the numbers speak a different language." Conversely, the WHO had been chalked up to "jumping the gun" in declaring a pandemic a few years earlier with swine flu. From March 9, 2020, the U.S. television network CNN used the term "pandemic" in its coverage. This was justified by senior medical correspondent Sanjay Gupta on the grounds that SARS-CoV-2 was spreading to every continent except Antarctica, that case numbers were rising persistently in several states, and that there was continued human-to-human transmission there. Gupta indicated that U.S. public health officials are already signaling a shift in strategy from containment to mitigation. These strategies are explained in the RKI Epidemiological Bulletin.
In light of rising infection figures outside China, WHO Director-General Tedros Adhanom Ghebreyesus said in his speech on Feb. 26, 2020, that declaring a pandemic was possible only after careful analysis of the facts, referring to the "international health emergency" already in effect since late January 2020 as WHO's highest alert level. He warned that careless use of the word pandemic could lead to unnecessary fears and stigmatization being reinforced, without any benefit to counteract this. Of course, he said, WHO would not hesitate to speak of a pandemic if that was the correct description of the situation. He repeated this statement in his March 2, 2020, speech, explaining that 90% of globally reported cases came from China and that 81% of the 8,739 cases of infection outside China occurred in four countries. On March 9, 2020 - at which time the number of infection cases was over 100,000, reported from over 100 countries - Ghebreyesus said that the threat of a pandemic was very real, but that it would be the first pandemic in history that could be controlled. On March 11, 2020, WHO officially declared the epidemic to date a pandemic, the first since Pandemic H1N1 in 2009-10, and Ghebreyesus referred to Europe as the "epicenter of the pandemic" in his March 13 speech. The reason he gave was that at that time there were more cases of infection and death in Europe than in the rest of the world, except China.
In a report published in May 2021, an independent expert commission appointed by the WHO stated that the WHO as well as governments had reacted too slowly to the pandemic. On this basis, it proposed a pandemic fund of five to ten billion dollars annually to finance precautions against a new pandemic.
Misinformation and conspiracy theories
→ Main article: Misinformation on the COVID-19 pandemic.
In the course of the COVID-19 pandemic, there was also an abundance of misinformation spread by private as well as government agencies of authoritarian states, which spread rapidly on social media. In reference to the rapid spread of the pandemic, the overload of information that is easily accessible online at the click of a button and spreads just as rapidly has been dubbed an "infodemic." It's often not just memes or videos that spread quickly, but also fake news and disinformation.
In the course of the controversies surrounding the assessment of the epidemic and then pandemic (especially with regard to its severity and danger) and consequently in the debate about the measures to be taken, there were also (especially at the beginning) many statements that downplayed the epidemic and in doing so did not acknowledge scientific findings, openly attacked them or ignored them. In Germany, these were prominently the former health politician Wolfgang Wodarg and the retired microbiologist Sucharit Bhakdi. In the U.S., influential in this direction were Richard A. Epstein (* 1943, law professor at the Hoover Institution) as well as members of the U.S. Senate and the U.S. government.
The Chinese government is accused of covering up the outbreak of the disease for a long time, wasting valuable time to contain it early. For example, doctors such as Li Wenliang in Wuhan who reported on the new disease were silenced, disinformation was spread about the origin, mode of transmission, and effects of SARS-CoV-2, and research institutions were ordered to stop testing. See also the Origin section above and the China section in the COVID-19 Pandemic Misinformation article.
In the Austrian ski resort of Ischgl, many vacationers became infected in the après-ski bars and cable cars there. Upon their return, infected vacationers and seasonal workers who had worked in Ischgl spread the virus throughout Europe. Local authorities are accused of not intervening for too long and spreading false facts about the infectivity of the virus. For example, the Tyrol Regional Sanitary Directorate claimed that it was "rather unlikely from a medical point of view" that a bartender who had contracted COVID-19 had infected guests in his bar. See also COVID-19 pandemic in Austria, Chronology section.
Weighing costs against benefits
→ Main article: Mass quarantine#Cost-benefit ratio
Potential impact on the rule of law and civil rights
Drastic measures to contain the spread of the virus, such as quarantine, isolation of particularly affected areas, spatial distancing, exit restrictions or entry bans, have often been accepted by the public as necessary, but have also been criticized in part as belated or even as questionable. Measures that undermine data protection and other legal bases also arouse concern. Sometimes the critical situation is a temptation for authoritarian politicians to establish corresponding structures.
At the end of March 2020, the European Commission warned against disproportionate political measures in response to the pandemic. EU Commission President Ursula von der Leyen stressed that such measures should not last indefinitely. In Hungary, the parliament passed an emergency law on March 30, 2020, allowing Prime Minister Viktor Orbán extensive special powers. He could rule by decree without a time limit and extend the state of emergency imposed on March 11, 2020, at will without parliamentary approval. No elections or referendums could be held during the state of emergency. Furthermore, the law increased penalties for violating quarantine regulations and spreading false news. Journalists feared that critical reports could lead to prison sentences of up to five years. Press comments accused the Hungarian prime minister of suspending the rule of law and disempowering parliament. World Medical Association President Frank Ulrich Montgomery spoke out against both exit restrictions and border closures ahead of March 18, also in light of Italian developments, saying they were "political actionism."
Virologist Jonas Schmidt-Chanasit recommends individual measures adapted to the respective healthcare system and situation and was critical of possible curfew restrictions and assembly bans because these promoted social stress, which could also trigger illness or even suicides. Michael Tsokos, professor of forensic medicine at Berlin's Charité hospital, reported cases in May 2020 of people taking their own lives because they were afraid of the consequences of the pandemic. This, he said, was a previously unknown phenomenon. He said that in none of these "corona suicides" had he found an infection, but all the victims had been psychologically preoccupied or ill. According to Tsokos, these suicides are an indicator of the strong insecurity of psychologically burdened people by politics and the media; he sees here the rights of a particularly weak population group violated, which has no lobby.
Historian René Schlott considers the "willingness, almost compliancy" with which temporary restrictions of fundamental rights such as freedom of assembly, freedom of trade or the right to asylum - through the previously rejected far-reaching closure of the EU's external borders - are accepted to be worrying. Children's rights would also be restricted if, for example, visits to the playground were prohibited. Criticism of this and the search for alternatives would be defamed, and instead authoritarian leadership would be demanded. Schlott sees the long-term habituation to such measures as problematic, and even fears that they could serve as a "script for a right-wing populist takeover." Critics consider Schlott's viewpoint to be ruthless individualism that can endanger lives at the expense of protecting at-risk groups and social solidarity in favor of one's own needs; harsh words on such views are spoken in Italy, for example.
Julia Leininger, head of Governance, Statehood, Security at the German Development Institute, called the COVID-19 pandemic a "fire accelerant for autocratization trends." When autocracies deploy social control without broad agreement on measures, it erodes public trust and social solidarity in the long run, he said. Leininger therefore called the protection and promotion of democracy the "order of the day" in international cooperation.
Ulrich Krökel analyzes in Zeit Online developments among some politicians also within the EU as "a temptation for authoritarians". Especially the "right-wing governments in Poland and Hungary", but also in Ukraine, according to Krökel, "discovered the corona virus for their own purposes. With the reference to China, they are trying to establish authoritarian structures ... The voices of the admonishers" were hardly heard "in the acute crisis situation.
Stefan Brink, data protection commissioner of the state of Baden-Württemberg, warned against "breaking the law" when dealing with infected persons. According to Brink, data protection is "often pushed aside". But if the state is not reliable in this area, he said, "it loses the trust it needs so that citizens will follow it." It is "extremely important that government agencies signal: Yes, we have an exceptional situation, but we abide by the law." In Israel, he said, the intelligence service uses "movement profiles of individual people to check compliance with quarantine regulations." In Austria, he said, "mobile phone providers offer their location data to the state." This was "a clear breach of telecommunications secrecy." It was not known whether "lists of infected or suspected cases have already been retrieved from health offices" in Germany. Later it became known that "the police" had indeed collected data of people "infected with the coronavirus" in "several federal states [...]".
Futurologist Sven Gábor Jánszky warns against holding on to the current restrictions in the long term. He says that overcoming the corona crisis is also about "ensuring that great achievements of our society such as democracy, freedom or self-determination [...] are not lost at the same time." The situation in which there are no serious counter-opinions to the thesis that politicians must listen above all to recognized virologists should not be allowed to last. In the long run, only a policy that systematically identifies infected people and isolates them from the rest of the population together with risk groups can succeed and count on the approval of the electorate.
See also: Protests in Germany during the COVID-19 pandemic and Legal assessment of the measures against the COVID-19 pandemic in Germany.
Debate on herd immunity through natural contamination
→ Main article: Herd immunity #Debate on herd immunity through natural contagion.

Locked playground in Stuttgart in March 2020
See also
![]()
Portal: COVID-19 - Overview of Wikipedia content related to COVID-19
- List of casualties of the COVID-19 pandemic
- List of epidemics and pandemics
- Pandemic Prevention
Questions and Answers
Q: What is the name of the virus that causes COVID-19?
A: The virus that causes COVID-19 is called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Q: How does SARS-CoV-2 spread from person to person?
A: SARS-CoV-2 spreads from one person to another through small drops made when coughing or sneezing, and it can also spread when people touch a surface with the virus and then touch their face.
Q: What are some common symptoms of COVID-19?
A: Common symptoms of COVID-19 include fever, cough, and difficulty breathing. In some cases, the illness can worsen with pneumonia and acute respiratory distress syndrome.
Q: Are there any antiviral medicines for COVID-19 available?
A: No antiviral medicine for COVID-19 is currently available; doctors usually provide supportive therapy instead.
Q: How can people avoid spreading the virus?
A: People can avoid spreading the virus by regularly washing their hands, covering their mouth when coughing, maintaining distance from other people, staying away from crowds, wearing medical or cloth face coverings, and quarantining if they think they are infected.
Q: Where did the outbreak start in December 2019?
A: The outbreak started in Wuhan, Hubei province in China in December 2019.
Q: How many vaccines have been approved as safe for use against COVID 19 so far?
A: As of January 2021, a number of vaccines for COVID 19 have been developed but only a few have been approved as safe for use. The first vaccine to be approved was created by Pfizer and BioNTech followed by Oxford/ AstraZeneca vaccine while 25 other vaccines have been approved by at least one country and many more are being developed.
Search within the encyclopedia

